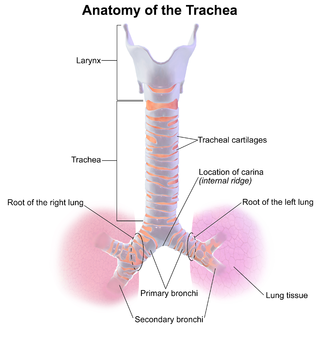
Tracheal intubation, usually simply referred to as intubation, is the placement of a flexible plastic tube into the trachea (windpipe) to maintain an open airway or to serve as a conduit through which to administer certain drugs. It is frequently performed in critically injured, ill, or anesthetized patients to facilitate ventilation of the lungs, including mechanical ventilation, and to prevent the possibility of asphyxiation or airway obstruction.
Tracheotomy, or tracheostomy, is a surgical airway management procedure which consists of making an incision (cut) on the anterior aspect (front) of the neck and opening a direct airway through an incision in the trachea (windpipe). The resulting stoma (hole) can serve independently as an airway or as a site for a tracheal tube or tracheostomy tube to be inserted; this tube allows a person to breathe without the use of the nose or mouth.
Pulmonary aspiration is the entry of material such as pharyngeal secretions, food or drink, or stomach contents from the oropharynx or gastrointestinal tract, into the larynx and lower respiratory tract, the portions of the respiratory system from the trachea (windpipe) to the lungs. A person may inhale the material, or it may be delivered into the tracheobronchial tree during positive pressure ventilation. When pulmonary aspiration occurs during eating and drinking, the aspirated material is often colloquially referred to as "going down the wrong pipe".

General anaesthesia (UK) or general anesthesia (US) is a method of medically inducing loss of consciousness that renders a patient unarousable even with painful stimuli. This effect is achieved by administering either intravenous or inhalational general anaesthetic medications, which often act in combination with an analgesic and neuromuscular blocking agent. Spontaneous ventilation is often inadequate during the procedure and intervention is often necessary to protect the airway. General anaesthesia is generally performed in an operating theater to allow surgical procedures that would otherwise be intolerably painful for a patient, or in an intensive care unit or emergency department to facilitate endotracheal intubation and mechanical ventilation in critically ill patients. Depending on the procedure, general anaesthesia may be optional or required. Regardless of whether a patient may prefer to be unconscious or not, certain pain stimuli could result in involuntary responses from the patient that may make an operation extremely difficult. Thus, for many procedures, general anaesthesia is required from a practical perspective.

Airway management includes a set of maneuvers and medical procedures performed to prevent and relieve airway obstruction. This ensures an open pathway for gas exchange between a patient's lungs and the atmosphere. This is accomplished by either clearing a previously obstructed airway; or by preventing airway obstruction in cases such as anaphylaxis, the obtunded patient, or medical sedation. Airway obstruction can be caused by the tongue, foreign objects, the tissues of the airway itself, and bodily fluids such as blood and gastric contents (aspiration).
Awareness under anesthesia, also referred to as intraoperative awareness or accidental awareness during general anesthesia (AAGA), is a rare complication of general anesthesia where patients regain varying levels of consciousness during their surgical procedures. While anesthesia awareness is possible without resulting in any long-term memory of the experience, it is also possible for victims to have awareness with explicit recall, where they can remember the events related to their surgery.
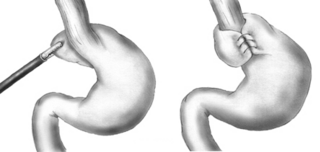
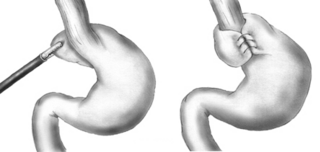
A Nissen fundoplication, or laparoscopic Nissen fundoplication when performed via laparoscopic surgery, is a surgical procedure to treat gastroesophageal reflux disease (GERD) and hiatal hernia. In GERD, it is usually performed when medical therapy has failed; but, with a Type II (paraesophageal) hiatus hernia, it is the first-line procedure. The Nissen fundoplication is total (360°), but partial fundoplications known as Thal, Belsey, Dor, Lind, and Toupet fundoplications are alternative procedures with somewhat different indications and outcomes.
In anaesthesia and advanced airway management, rapid sequence induction (RSI) – also referred to as rapid sequence intubation or as rapid sequence induction and intubation (RSII) or as crash induction – is a special process for endotracheal intubation that is used where the patient is at a high risk of pulmonary aspiration. It differs from other techniques for inducing general anesthesia in that several extra precautions are taken to minimize the time between giving the induction drugs and securing the tube, during which period the patient's airway is essentially unprotected.
Stridor is an extra-thoracic high-pitched breath sound resulting from turbulent air flow in the larynx or lower in the bronchial tree. It is different from a stertor, which is a noise originating in the pharynx.
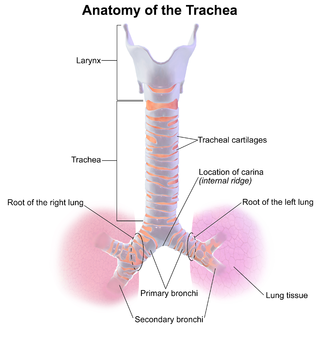
Tracheitis is an inflammation of the trachea. Although the trachea is usually considered part of the lower respiratory tract, in ICD-10 tracheitis is classified under "acute upper respiratory infections".

Laryngeal papillomatosis, also known as recurrent respiratory papillomatosis (RRP) or glottal papillomatosis, is a rare medical condition in which benign tumors (papilloma) form along the aerodigestive tract. There are two variants based on the age of onset: juvenile and adult laryngeal papillomatosis. The tumors are caused by human papillomavirus (HPV) infection of the throat. The tumors may lead to narrowing of the airway, which may cause vocal changes or airway obstruction. Laryngeal papillomatosis is initially diagnosed through indirect laryngoscopy upon observation of growths on the larynx and can be confirmed through a biopsy. Treatment for laryngeal papillomatosis aims to remove the papillomas and limit their recurrence. Due to the recurrent nature of the virus, repeated treatments usually are needed. Laryngeal papillomatosis is primarily treated surgically, though supplemental nonsurgical and/or medical treatments may be considered in some cases. The evolution of laryngeal papillomatosis is highly variable. Though total recovery may be observed, it is often persistent despite treatment. The number of new cases of laryngeal papillomatosis cases is approximately 4.3 cases per 100,000 children and 1.8 cases per 100,000 adults annually.
Mendelson's syndrome, named in 1946 for American obstetrician and cardiologist Curtis Lester Mendelson, is a form of chemical pneumonitis or aspiration pneumonitis caused by aspiration of stomach contents during anaesthesia in childbirth. This complication of anaesthesia led, in part, to the longstanding nil per os recommendation for women in labour.

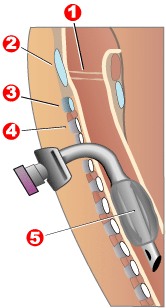
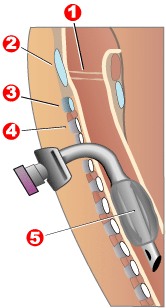
The Combitube—also known as the esophageal tracheal airway or esophageal tracheal double-lumen airway—is a blind insertion airway device (BIAD) used in the pre-hospital and emergency setting. It is designed to provide an airway to facilitate the mechanical ventilation of a patient in respiratory distress.

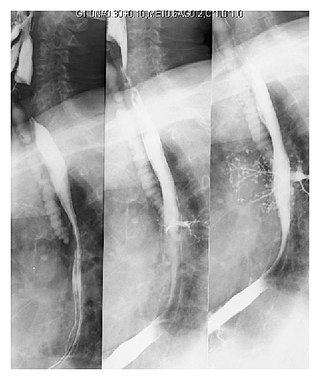
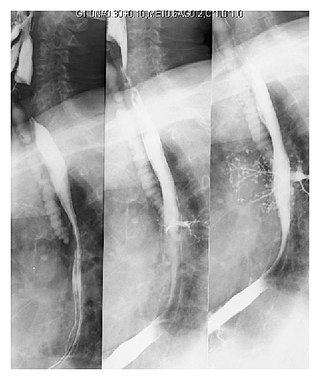
Bronchoscopy is an endoscopic technique of visualizing the inside of the airways for diagnostic and therapeutic purposes. An instrument (bronchoscope) is inserted into the airways, usually through the nose or mouth, or occasionally through a tracheostomy. This allows the practitioner to examine the patient's airways for abnormalities such as foreign bodies, bleeding, tumors, or inflammation. Specimens may be taken from inside the lungs. The construction of bronchoscopes ranges from rigid metal tubes with attached lighting devices to flexible optical fiber instruments with realtime video equipment.

Neurocritical care is a medical field that treats life-threatening diseases of the nervous system and identifies, prevents, and treats secondary brain injury.

Laryngopharyngeal reflux (LPR) or laryngopharyngeal reflux disease (LPRD) is the retrograde flow of gastric contents into the larynx, oropharynx and/or the nasopharynx. LPR causes respiratory symptoms such as cough and wheezing and is often associated with head and neck complaints such as dysphonia, globus pharyngis, and dysphagia. LPR may play a role in other diseases, such as sinusitis, otitis media, and rhinitis, and can be a comorbidity of asthma. While LPR is commonly used interchangeably with gastroesophageal reflux disease (GERD), it presents with a different pathophysiology.

Tracheobronchial injury is damage to the tracheobronchial tree. It can result from blunt or penetrating trauma to the neck or chest, inhalation of harmful fumes or smoke, or aspiration of liquids or objects.
Vocal cord dysfunction (VCD) is a pathology affecting the vocal folds characterized by full or partial vocal fold closure causing difficulty and distress during respiration, especially during inhalation.

Foreign body aspiration occurs when a foreign body enters the airway which can cause difficulty breathing or choking. Objects may reach the respiratory tract and the digestive tract from the mouth and nose, but when an object enters the respiratory tract it is termed aspiration. The foreign body can then become lodged in the trachea or further down the respiratory tract such as in a bronchus. Regardless of the type of object, any aspiration can be a life-threatening situation and requires timely recognition and action to minimize risk of complications. While advances have been made in management of this condition leading to significantly improved clinical outcomes, there were still 2,700 deaths resulting from foreign body aspiration in 2018. Approximately one child dies every five days due to choking on food in the United States, highlighting the need for improvements in education and prevention.
Negative-pressure pulmonary edema (NPPE), also known as Postobstructive Pulmonary Edema, is a clinical phenomenon that results from the generation of large negative pressures in the airways during attempted inspiration against some form of obstruction of the upper airways. The most common reported cause of NPPE reported in adults is laryngospasm, while the most implicated causes in children are infectious croup and epiglottitis. The large negative pressures created in the airways by inhalation against an upper airway obstruction can lead to fluid being drawn from blood vessels supplying the lungs into the alveoli, causing pulmonary edema and impaired ability for oxygen exchange (hypoxemia). The main treatment for NPPE is supportive care in an intensive care unit and can be fatal without intervention.