Treatment of foreign body aspiration is determined by the age of the patient and the severity of obstruction of the airway involved. [21]
Basic management
An airway obstruction can be partial or complete. In partial obstruction, the patient can usually clear the foreign body with coughing. [21] In complete obstruction, acute intervention is required to remove the foreign body. [21]
If foreign body aspiration is suspected, finger sweeping in the mouth is not recommended due to the increased risk of displacing the foreign object further into the airway. [21]
For choking children less than 1 year of age, the child should be placed face down over the rescuer's arm. [21] Back blows should be delivered with the heel of the hand, then the patient should be turned face-up and chest thrusts should be administered. [21] The rescuer should alternate five back blows followed by five chest thrusts until the object is cleared. [21] The Heimlich maneuver should be used in choking patients older than 1 year of age to dislodge a foreign body. [21] If the patient becomes unresponsive during physical intervention, cardiopulmonary resuscitation (CPR) should be started. [21]
Advanced management
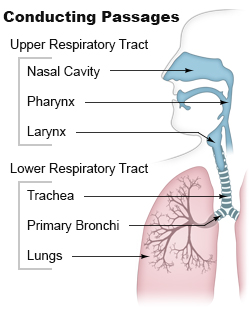
In the event that the basic measures do not remove the foreign body, and adequate ventilation cannot be restored, need for treatment by trained personnel becomes necessary. [21] Laryngoscopy should be performed in unresponsive patients if non-invasive airway clearance techniques are unsuccessful. [22] Laryngoscopy involves placing a device in the mouth to visualize the back of the airway. [22] If the foreign body can be seen, it can be removed with forceps. [22] An endotracheal tube should then be placed in order to prevent airway compromise from resulting inflammation after the procedure. [22] If the foreign body cannot be visualized, intubation, tracheotomy, or needle cricothyrotomy can be done to restore an airway for patients who have become unresponsive due to airway compromise. [21]
If non-invasive measures do not dislodge the foreign body, and the patient can maintain adequate ventilation, rigid bronchoscopy under general anesthesia should be performed. [21] Supplemental oxygen, cardiac monitoring, and a pulse oximeter should be applied to the patient. [22] Efforts should be made to keep the patient calm and avoid agitating the patient to prevent further airway compromise. [22] Flexible rather than rigid bronchoscopy might be used when the diagnosis or object location are unclear. When flexible bronchoscope is used, rigid bronchoscope is typically on standby and readily available as this is the preferred approach for removal. [23] Rigid bronchoscopy allows good airway control, ready bleeding management, better visualization, and ability to manipulate the aspirated object with a variety of forceps. [23] Flexible bronchoscopy may be used for extraction when distal access is needed and the operator is experienced in this technique. [23] Potential advantages include avoidance of general anesthesia as well as the ability to reach subsegmental bronchi which are smaller in diameter and further down the respiratory tract than the main bronchi. [23] The main disadvantage of using a flexible scope is the risk of further dislodging the object and causing airway compromise. [23] Bronchoscopy is successful in removing the foreign body in approximately 95% of cases with a complication rate of only 1%. [23]
After the foreign body is removed, patients should receive nebulized beta-adrenergic medication and chest physiotherapy to further protect the airway. [21] Steroidal anti-inflammatories and antibiotics are not routinely administered except in certain scenarios. [21] These include situations such as when the foreign body is difficult or impossible to extract, when there is a documented respiratory tract infection, and when swelling within the airway occurs after removal of the object. [23] Glucocorticoids may be administered when the foreign body is surrounded by inflamed tissue and extraction is difficult or impossible. [23] In such cases, extraction may be delayed for a short course of glucocorticoids so that the inflammation may be reduced before subsequent attempts. [23] These patients should remain under observation in the hospital until successful extraction as this practice can result in dislodgement of the foreign body. [23] Antibiotics are appropriate when an infection has developed but should not delay extraction. [23] In fact, removal of the object may improve infection control by removing the infectious source as well as using cultures taken during the bronchoscopy to guide antibiotic choice. [23] When airway edema or swelling occur, the patient may have stridor. In these cases, glucocorticoids, aerosolized epinephrine, or helium oxygen therapy may be considered as part of the management plan. [23]
Patients who are clinically stable with no need for supplemental oxygen after extraction may be discharged from the hospital the same day as the procedure. [24] Routine imaging such as a follow-up chest x-ray are not needed unless symptoms persist or worsen, or if the patient had imaging abnormalities previously to verify return to normal. [24] Most children are discharged within 24 hours of the procedure. [25]