Related Research Articles

Intensive care medicine, also called critical care medicine, is a medical specialty that deals with seriously or critically ill patients who have, are at risk of, or are recovering from conditions that may be life-threatening. It includes providing life support, invasive monitoring techniques, resuscitation, and end-of-life care. Doctors in this specialty are often called intensive care physicians, critical care physicians, or intensivists.

Acute respiratory distress syndrome (ARDS) is a type of respiratory failure characterized by rapid onset of widespread inflammation in the lungs. Symptoms include shortness of breath (dyspnea), rapid breathing (tachypnea), and bluish skin coloration (cyanosis). For those who survive, a decreased quality of life is common.
Prognosis is a medical term for predicting the likelihood or expected development of a disease, including whether the signs and symptoms will improve or worsen or remain stable over time; expectations of quality of life, such as the ability to carry out daily activities; the potential for complications and associated health issues; and the likelihood of survival. A prognosis is made on the basis of the normal course of the diagnosed disease, the individual's physical and mental condition, the available treatments, and additional factors. A complete prognosis includes the expected duration, function, and description of the course of the disease, such as progressive decline, intermittent crisis, or sudden, unpredictable crisis.
Systemic inflammatory response syndrome (SIRS) is an inflammatory state affecting the whole body. It is the body's response to an infectious or noninfectious insult. Although the definition of SIRS refers to it as an "inflammatory" response, it actually has pro- and anti-inflammatory components.
APACHE II is a severity-of-disease classification system, one of several ICU scoring systems. It is applied within 24 hours of admission of a patient to an intensive care unit (ICU): an integer score from 0 to 71 is computed based on several measurements; higher scores correspond to more severe disease and a higher risk of death. The first APACHE model was presented by Knaus et al. in 1981.
An induced coma – also known as a medically induced coma (MIC), barbiturate-induced coma, or drug-induced coma – is a temporary coma brought on by a controlled dose of an anesthetic drug, often a barbiturate such as pentobarbital or thiopental. Other intravenous anesthetic drugs such as midazolam or propofol may be used.

A pulmonary artery catheter (PAC), also known as a Swan-Ganz catheter or right heart catheter, is a balloon-tipped catheter that is inserted into a pulmonary artery in a procedure known as pulmonary artery catheterization or right heart catheterization. Pulmonary artery catheterization is a useful measure of the overall function of the heart particularly in those with complications from heart failure, heart attack, arrythmias or pulmonary embolism. It is also a good measure for those needing intravenous fluid therapy, for instance post heart surgery, shock, and severe burns. The procedure can also be used to measure pressures in the heart chambers.
Stress hyperglycemia is a medical term referring to transient elevation of the blood glucose due to the stress of illness. It usually resolves spontaneously, but must be distinguished from various forms of diabetes mellitus.
The sequential organ failure assessment score, previously known as the sepsis-related organ failure assessment score, is used to track a person's status during the stay in an intensive care unit (ICU) to determine the extent of a person's organ function or rate of failure. The score is based on six different scores, one each for the respiratory, cardiovascular, hepatic, coagulation, renal and neurological systems.
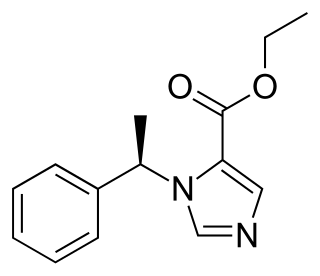
Etomidate is a short-acting intravenous anaesthetic agent used for the induction of general anaesthesia and sedation for short procedures such as reduction of dislocated joints, tracheal intubation, cardioversion and electroconvulsive therapy. It was developed at Janssen Pharmaceutica in 1964 and was introduced as an intravenous agent in 1972 in Europe and in 1983 in the United States.
In statistical hypothesis testing, a type I error is the mistaken rejection of an actually true null hypothesis, while a type II error is the failure to reject a null hypothesis that is actually false. Much of statistical theory revolves around the minimization of one or both of these errors, though the complete elimination of either is a statistical impossibility if the outcome is not determined by a known, observable causal process. By selecting a low threshold (cut-off) value and modifying the alpha (α) level, the quality of the hypothesis test can be increased. The knowledge of type I errors and type II errors is widely used in medical science, biometrics and computer science.
The Surviving Sepsis Campaign (SSC) is a global initiative to bring together professional organizations in reducing mortality from sepsis. The purpose of the SSC is to create an international collaborative effort to improve the treatment of sepsis and reduce the high mortality rate associated with the condition. The Surviving Sepsis Campaign and the Institute for Healthcare Improvement have teamed up to achieve a 25 percent reduction in sepsis mortality by 2009. The guidelines were updated in 2016 and again in 2021.
The Arctic Sun Temperature Management System is a non-invasive targeted temperature management system. It modulates patient temperature by circulating chilled water in pads directly adhered to the patient's skin. Using varying water temperatures and a computer algorithm, a patient's body temperature can be better controlled. It is produced by Medivance, Inc. of Louisville, Colorado.
Critical illness–related corticosteroid insufficiency is a form of adrenal insufficiency in critically ill patients who have blood corticosteroid levels which are inadequate for the severe stress response they experience. Combined with decreased glucocorticoid receptor sensitivity and tissue response to corticosteroids, this adrenal insufficiency constitutes a negative prognostic factor for intensive care patients.

A pediatric intensive care unit, usually abbreviated to PICU, is an area within a hospital specializing in the care of critically ill infants, children, teenagers, and young adults aged 0-21. A PICU is typically directed by one or more pediatric intensivists or PICU consultants and staffed by doctors, nurses, and respiratory therapists who are specially trained and experienced in pediatric intensive care. The unit may also have nurse practitioners, physician assistants, physiotherapists, social workers, child life specialists, and clerks on staff, although this varies widely depending on geographic location. The ratio of professionals to patients is generally higher than in other areas of the hospital, reflecting the acuity of PICU patients and the risk of life-threatening complications. Complex technology and equipment is often in use, particularly mechanical ventilators and patient monitoring systems. Consequently, PICUs have a larger operating budget than many other departments within the hospital.

Placebo-controlled studies are a way of testing a medical therapy in which, in addition to a group of subjects that receives the treatment to be evaluated, a separate control group receives a sham "placebo" treatment which is specifically designed to have no real effect. Placebos are most commonly used in blinded trials, where subjects do not know whether they are receiving real or placebo treatment. Often, there is also a further "natural history" group that does not receive any treatment at all.
The minimal important difference (MID) or minimal clinically important difference (MCID) is the smallest change in a treatment outcome that an individual patient would identify as important and which would indicate a change in the patient's management.
Post-intensive care syndrome (PICS) describes a collection of health disorders that are common among patients who survive critical illness and intensive care. Generally, PICS is considered distinct from the impairments experienced by those who survive critical illness and intensive care following traumatic brain injury and stroke. The range of symptoms that PICS describes falls under three broad categories: physical impairment, cognitive impairment, and psychiatric impairment. A person with PICS may have symptoms from one or multiple of these categories.

Vasopressin infusions are in use for septic shock patients not responding to fluid resuscitation or infusions of catecholamines to increase the blood pressure while sparing the use of catecholamines. These argipressins have much shorter elimination half-life than synthetic non-arginine vasopresines with much longer elimination half-life of many hours. Further, argipressins act on V1a, V1b, and V2 receptors which consequently lead to higher eGFR and lower vascular resistance in the lungs. A number of injectable arginine vasopressins are in clinical use in the United States and the European Union. Pitressin among others, is a medication most commonly used in the treatment of frequent urination, increased thirst, and dehydration such as that resulting from diabetes insipidus, which causes increased and diluted urine. It is used to treat abdominal distension following some surgeries, and in stomach roentgenography. Vasopressin is a hormone that affects the kidneys and reduces urine flow.
Clinicians routinely check the pupils of critically injured and ill patients to monitor neurological status. However, manual pupil measurements have been shown to be subjective, inaccurate, and not repeatable or consistent. Automated assessment of the pupillary light reflex has emerged as an objective means of measuring pupillary reactivity across a range of neurological diseases, including stroke, traumatic brain injury and edema, tumoral herniation syndromes, and sports or war injuries. Automated pupillometers are used to assess an array of objective pupillary variables including size, constriction velocity, latency, and dilation velocity, which are normalized and standardized to compute an indexed score such as the Neurological Pupil index (NPi).
References
- 1 2 Walsh M, et al. (June 1, 2014), "The statistical significance of randomized controlled trial results is frequently fragile: a case for a Fragility Index", Journal of Clinical Epidemiology (in German), vol. 67, no. 6, pp. 622–628, doi: 10.1016/j.jclinepi.2013.10.019 , retrieved 2018-05-10
- ↑ Ridgeon EE, et al. (July 2016), "The Fragility Index in Multicenter Randomized Controlled Critical Care Trials", Critical Care Medicine, vol. 44, no. 7, pp. 1278–84, doi:10.1097/CCM.0000000000001670, PMID 26963326
- ↑ Boyd, Owen (July 2016), "The Fragility of Evidence in Critical Care Research: Is It Just a House of Cards?", Critical Care Medicine, vol. 44, no. 7, pp. 1423–4, doi:10.1097/CCM.0000000000001756