Related Research Articles
Medicare is the publicly funded universal health care insurance scheme in Australia operated by the nation's social security agency, Services Australia. The scheme either partially or fully covers the cost of most health care, with services being delivered by state and territory governments or private enterprises. All Australian citizens and permanent residents are eligible to enrol in Medicare, as well as international visitors from 11 countries that have reciprocal agreements for medically necessary treatment.

A general practitioner (GP) or family physician is a doctor who is a consultant in general practice.
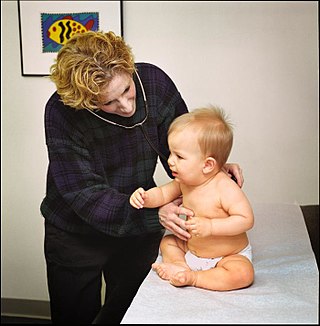
General practice is personal, family, and community-orientated comprehensive primary care that includes diagnosis, continues over time and is anticipatory as well as responsive.

Family medicine is a medical specialty within primary care that provides continuing and comprehensive health care for the individual and family across all ages, genders, diseases, and parts of the body. The specialist, who is usually a primary care physician, is named a family physician. It is often referred to as general practice and a practitioner as a general practitioner. Historically, their role was once performed by any doctor with qualifications from a medical school and who works in the community. However, since the 1950s, family medicine / general practice has become a specialty in its own right, with specific training requirements tailored to each country. The names of the specialty emphasize its holistic nature and/or its roots in the family. It is based on knowledge of the patient in the context of the family and the community, focusing on disease prevention and health promotion. According to the World Organization of Family Doctors (WONCA), the aim of family medicine is "promoting personal, comprehensive and continuing care for the individual in the context of the family and the community". The issues of values underlying this practice are usually known as primary care ethics.

Medical education in Australia includes the educational activities involved in the initial and ongoing training of Medical Practitioners. In Australia, medical education begins in Medical School; upon graduation it is followed by a period of pre-vocational training including Internship and Residency; thereafter, enrolment into a specialist-vocational training program as a Registrar eventually leads to fellowship qualification and recognition as a fully qualified Specialist Medical Practitioner. Medical education in Australia is facilitated by Medical Schools and the Medical Specialty Colleges, and is regulated by the Australian Medical Council (AMC) and Australian Health Practitioner Regulation Agency (AHPRA) of which includes the Medical Board of Australia where medical practitioners are registered nationally.
Polyclinics in England were intended to offer a greater range of services than were offered by current general practitioner (GP) practices and local health centres. In addition to traditional GP services they would offer extended urgent care, healthy living services, community mental health services and social care, whilst being more accessible and less medicalised than hospitals. A variety of models were proposed, ranging from networks of existing clinics to larger premises with several colocated general practitioner (GP) practices, more extensive facilities and additional services provided by allied healthcare professionals.

The Royal Australian College of General Practitioners (RACGP) is the professional body for general practitioners (GPs) in Australia. The RACGP is responsible for maintaining standards for quality clinical practice, education and training, and research in Australian general practice. The RACGP represents over 40,000 members across metropolitan, urban, rural and remote Australia.
General medical services (GMS) is the range of healthcare that is provided by general practitioners as part of the National Health Service in the United Kingdom. The NHS specifies what GPs, as independent contractors, are expected to do and provides funding for this work through arrangements known as the General Medical Services Contract. Today, the GMS contract is a UK-wide arrangement with minor differences negotiated by each of the four UK health departments. In 2013 60% of practices had a GMS contract as their principal contract. The contract has sub-sections and not all are compulsory. The other forms of contract are the Personal Medical Services or Alternative Provider Medical Services contracts. They are designed to encourage practices to offer services over and above the standard contract. Alternative Provider Medical Services contracts, unlike the other contracts, can be awarded to anyone, not just GPs, don't specify standard essential services, and are time limited. A new contract is issued each year.

NHS Scotland, sometimes styled NHSScotland, is the publicly–funded healthcare system in Scotland and one of the four systems that make up the National Health Service in the United Kingdom. It operates 14 territorial NHS boards across Scotland, supported by seven special non-geographic health boards, and Public Health Scotland.
Health and Social Care is the publicly funded healthcare system in Northern Ireland. Although having been created separately to the National Health Service (NHS), it is nonetheless considered a part of the overall national health service in the United Kingdom. The Northern Ireland Executive through its Department of Health is responsible for its funding, while the Public Health Agency is the executive agency responsible for the provision of public health and social care services across Northern Ireland. It is free of charge to all citizens of Northern Ireland and the rest of the United Kingdom.
A patient safety organization (PSO) is a group, institution, or association that improves medical care by reducing medical errors. Common functions of patient safety organizations are data collection, analysis, reporting, education, funding, and advocacy. A PSO differs from a Federally designed Patient Safety Organization (PSO), which provides health care providers in the U.S. privilege and confidentiality protections for efforts to improve patient safety and the quality of patient care delivery
The Clinical Practice Research Datalink (CPRD) is an observational and interventional research service that operates as part of the UK Department of Health. It is jointly funded by the National Institute for Health and Care Research(NIHR) and the Medicines and Healthcare products Regulatory Agency (MHRA). CPRD is working closely with the extensive primary care, topic specific and comprehensive NIHR research networks and with NHS Digital.
Healthcare in England is mainly provided by the National Health Service (NHS), a public body that provides healthcare to all permanent residents in England, that is free at the point of use. The body is one of four forming the UK National Health Service as health is a devolved matter; there are differences with the provisions for healthcare elsewhere in the United Kingdom, and in England it is overseen by NHS England. Though the public system dominates healthcare provision in England, private health care and a wide variety of alternative and complementary treatments are available for those willing and able to pay.

Michael David Dixon, is an English general practitioner and current Head of the Royal Medical Household. He is Chair of The College of Medicine and Integrated Health and Visiting Professor at the University of Westminster.

Clinical commissioning groups (CCGs) were National Health Service (NHS) organisations set up by the Health and Social Care Act 2012 to organise the delivery of NHS services in each of their local areas in England. On 1 July 2022 they were abolished, and replaced by Integrated care systems as a result of the Health and Care Act 2022.
Healthcare in London, which consumes about a fifth of the NHS budget in England, is in many respects distinct from that in the rest of the United Kingdom, or England.
EMIS Health, formerly known as Egton Medical Information Systems, supplies electronic patient record systems and software used in primary care, acute care and community pharmacy in the United Kingdom. The company is based in Leeds. It claims that more than half of GP practices across the UK use EMIS Health software and holds number one or two market positions in its main markets. In June 2022 the company was acquired by Bordeaux UK Holdings II Limited, an affiliate of UnitedHealth's Optum business for a 49% premium on EMIS's closing share price.
Professor Nick Harding OBE BSc FRCGP FRCP HonMFPH DRCOG DOccMed PGDIP (Cardiology) SFFLM, born 21 December 1969, is a British general practitioner and Chief Medical Officer at Operose Health.
GP Federations became popular among English general practitioners after 2010 as a means to exploit the opportunities—or mitigate the threats—posed by the Five Year Forward View proposals in the English NHS which envisaged delivering primary care at a larger scale than the traditional GP list. It is widely believed that ‘Practices cannot survive on their own – they have to look at ways of making themselves stronger.’ 15 sites were selected in December 2015 to test new enhanced primary care models serving populations of 30,000 to 50,000 patients. Some, but by no means all, clinical commissioning groups have given financial support to encourage the formation of federations.
A Primary care network is a structure which brings general practitioners together on an area basis, possibly with other clinicians, to address chronic disease management and prevention. In 2022 the term is used in England, Singapore and Alberta.
References
- ↑ "GP Liaisons". Te Whatu ora, Health New Zealand, Waitemata. Retrieved 21 June 2024.
- ↑ "GP Liaison Service". Peninsula Private Hospital, Ramsay Health. Retrieved 21 June 2024.
- ↑ "GP Liaison Unit". The Royal Women's Hospital Victoria, Australia. Retrieved 21 June 2024.
- ↑ "GP Liaison Office". Epsom and St. Helier University Hospitals, NHS Trust. Retrieved 21 June 2024.
- ↑ "Enhancing Integration: The General Practice Liaison Officer Model" (PDF). Queensland General Practice Liaison (QGPL) Network. Retrieved 21 June 2024.
- ↑ "GP and Primary Care Unit". Department of Health, Tasmanian Government. Retrieved 21 June 2024.
- ↑ "QGPL". Queensland General Practice Liaison Network. Retrieved 21 June 2024.
- ↑ "GP liaison officers boost primary care connections". InSight+, Medical Journal of Australia. Retrieved 21 June 2024.
- ↑ "General Practice Liaison". Metro North Health. Retrieved 21 June 2024.