Related Research Articles

A goitre, or goiter, is a swelling in the neck resulting from an enlarged thyroid gland. A goitre can be associated with a thyroid that is not functioning properly.

Hyperthyroidism is the condition that occurs due to excessive production of thyroid hormones by the thyroid gland. Thyrotoxicosis is the condition that occurs due to excessive thyroid hormone of any cause and therefore includes hyperthyroidism. It is noted that thyrotoxicosis is related to hyper-kinetic movement disorders including chorea and myoclonus. Some, however, use the terms interchangeably. Signs and symptoms vary between people and may include irritability, muscle weakness, sleeping problems, a fast heartbeat, heat intolerance, diarrhea, enlargement of the thyroid, hand tremor, and weight loss. Symptoms are typically less severe in the elderly and during pregnancy. An uncommon complication is thyroid storm in which an event such as an infection results in worsening symptoms such as confusion and a high temperature and often results in death. The opposite is hypothyroidism, when the thyroid gland does not make enough thyroid hormone.

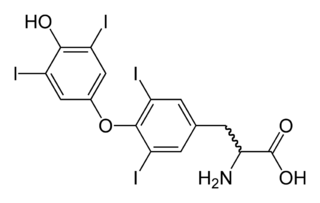
The thyroid, or thyroid gland, is an endocrine gland in vertebrates. In humans it is in the neck and consists of two connected lobes. The lower two thirds of the lobes are connected by a thin band of tissue called the thyroid isthmus. The thyroid is located at the front of the neck, below the Adam's apple. Microscopically, the functional unit of the thyroid gland is the spherical thyroid follicle, lined with follicular cells (thyrocytes), and occasional parafollicular cells that surround a lumen containing colloid. The thyroid gland secretes three hormones: the two thyroid hormones – triiodothyronine (T3) and thyroxine (T4) – and a peptide hormone, calcitonin. The thyroid hormones influence the metabolic rate and protein synthesis, and in children, growth and development. Calcitonin plays a role in calcium homeostasis. Secretion of the two thyroid hormones is regulated by thyroid-stimulating hormone (TSH), which is secreted from the anterior pituitary gland. TSH is regulated by thyrotropin-releasing hormone (TRH), which is produced by the hypothalamus.

Graves' disease, also known as toxic diffuse goiter, is an autoimmune disease that affects the thyroid. It frequently results in and is the most common cause of hyperthyroidism. It also often results in an enlarged thyroid. Signs and symptoms of hyperthyroidism may include irritability, muscle weakness, sleeping problems, a fast heartbeat, poor tolerance of heat, diarrhea and unintentional weight loss. Other symptoms may include thickening of the skin on the shins, known as pretibial myxedema, and eye bulging, a condition caused by Graves' ophthalmopathy. About 25 to 80% of people with the condition develop eye problems.
Hypothyroidism is a disorder of the endocrine system in which the thyroid gland does not produce enough thyroid hormone. It can cause a number of symptoms, such as poor ability to tolerate cold, a feeling of tiredness, constipation, slow heart rate, depression, and weight gain. Occasionally there may be swelling of the front part of the neck due to goiter. Untreated cases of hypothyroidism during pregnancy can lead to delays in growth and intellectual development in the baby or congenital iodine deficiency syndrome.

Myxedema is a term used synonymously with severe hypothyroidism. However, the term is also used to describe a dermatological change that can occur in hyperthyroidism and (rare) paradoxical cases of hypothyroidism. In this latter sense, myxedema refers to deposition of mucopolysaccharides in the dermis, which results in swelling of the affected area. One manifestation of myxedema occurring in the lower limb is pretibial myxedema, a hallmark of Graves disease, an autoimmune form of hyperthyroidism. Myxedema can also occur in Hashimoto thyroiditis and other long-standing forms of hypothyroidism.

Hashimoto's thyroiditis, also known as chronic lymphocytic thyroiditis and Hashimoto's disease, is an autoimmune disease in which the thyroid gland is gradually destroyed. Early on, symptoms may not be noticed. Over time, the thyroid may enlarge, forming a painless goiter. Some people eventually develop hypothyroidism with accompanying weight gain, fatigue, constipation, depression, hair loss, and general pains. After many years the thyroid typically shrinks in size. Potential complications include thyroid lymphoma. Furthermore, because it is common for untreated patients of Hashimoto’s to develop hypothyroidism, further complications can include, but are not limited to, high cholesterol, heart disease, heart failure, high blood pressure, myxedema, and potential pregnancy problems.
Ord's thyroiditis is a common form of thyroiditis, an autoimmune disease where the body's own antibodies fight the cells of the thyroid.

Thyroid disease is a medical condition that affects the function of the thyroid gland. The thyroid gland is located at the front of the neck and produces thyroid hormones that travel through the blood to help regulate many other organs, meaning that it is an endocrine organ. These hormones normally act in the body to regulate energy use, infant development, and childhood development.

Thyroiditis is the inflammation of the thyroid gland. The thyroid gland is located on the front of the neck below the laryngeal prominence, and makes hormones that control metabolism.

De Quervain's thyroiditis, also known as subacute granulomatous thyroiditis or giant cell thyroiditis, is a member of the group of thyroiditis conditions known as resolving thyroiditis. People of all ages and genders may be affected.

Graves’ ophthalmopathy, also known as thyroid eye disease (TED), is an autoimmune inflammatory disorder of the orbit and periorbital tissues, characterized by upper eyelid retraction, lid lag, swelling, redness (erythema), conjunctivitis, and bulging eyes (exophthalmos). It occurs most commonly in individuals with Graves' disease, and less commonly in individuals with Hashimoto's thyroiditis, or in those who are euthyroid.

Endocrine diseases are disorders of the endocrine system. The branch of medicine associated with endocrine disorders is known as endocrinology.
Postpartum thyroiditis refers to thyroid dysfunction occurring in the first 12 months after pregnancy and may involve hyperthyroidism, hypothyroidism or the two sequentially. According to the National Institute of Health, postpartum thyroiditis affects about 8% of pregnancies. There are, however, different rates reported globally. This is likely due to the differing amounts of average postpartum follow times around the world, and due to our own innate differences. For example, in Bangkok, Thailand the rate is 1.1%, but in Brazil it is 13.3%. The first phase is typically hyperthyroidism. Then, the thyroid either returns to normal or a woman develops hypothyroidism. Of those women who experience hypothyroidism associated with postpartum thyroiditis, one in five will develop permanent hypothyroidism requiring lifelong treatment.
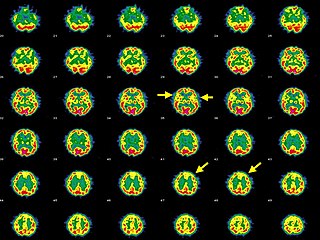
Hashimoto's encephalopathy, also known as steroid-responsive encephalopathy associated with autoimmune thyroiditis (SREAT), is a neurological condition characterized by encephalopathy, thyroid autoimmunity, and good clinical response to corticosteroids. It is associated with Hashimoto's thyroiditis, and was first described in 1966. It is sometimes referred to as a neuroendocrine disorder, although the condition's relationship to the endocrine system is widely disputed. It is recognized as a rare disease by the NIH Genetic and Rare Diseases Information Center.
Thyrotoxicosis factitia refers to a condition of thyrotoxicosis caused by the ingestion of exogenous thyroid hormone. It can be the result of mistaken ingestion of excess drug, such as levothyroxine and triiodothyronine, or as a symptom of Munchausen syndrome. It is an uncommon form of hyperthyroidism.
Autoimmune thyroiditis, is a chronic disease in which the body interprets the thyroid glands and its hormone products T3, T4 and TSH as threats, therefore producing special antibodies that target the thyroid's cells, thereby destroying it. It may present with hypothyroidism or hyperthyroidism and with or without a goiter.
Thyroid disease in pregnancy can affect the health of the mother as well as the child before and after delivery. Thyroid disorders are prevalent in women of child-bearing age and for this reason commonly present as a pre-existing disease in pregnancy, or after childbirth. Uncorrected thyroid dysfunction in pregnancy has adverse effects on fetal and maternal well-being. The deleterious effects of thyroid dysfunction can also extend beyond pregnancy and delivery to affect neurointellectual development in the early life of the child. Due to an increase in thyroxine binding globulin, an increase in placental type 3 deioidinase and the placental transfer of maternal thyroxine to the fetus, the demand for thyroid hormones is increased during pregnancy. The necessary increase in thyroid hormone production is facilitated by high human chorionic gonadotropin (hCG) concentrations, which bind the TSH receptor and stimulate the maternal thyroid to increase maternal thyroid hormone concentrations by roughly 50%. If the necessary increase in thyroid function cannot be met, this may cause a previously unnoticed (mild) thyroid disorder to worsen and become evident as gestational thyroid disease. Currently, there is not enough evidence to suggest that screening for thyroid dysfunction is beneficial, especially since treatment thyroid hormone supplementation may come with a risk of overtreatment. After women give birth, about 5% develop postpartum thyroiditis which can occur up to nine months afterwards. This is characterized by a short period of hyperthyroidism followed by a period of hypothyroidism; 20–40% remain permanently hypothyroid.
The signs and symptoms of Graves' disease generally result from the direct and indirect effects of hyperthyroidism ; exceptions are caused by the autoimmune processes of Graves' disease, such as Graves' ophthalmopathy, goitre and pretibial myxedema. These clinical manifestations can involve virtually every system in the body. The mechanisms that mediate these effects are not well understood. The severity of the signs and symptoms of hyperthyroidism is related to the duration of the disease, the magnitude of the thyroid hormone excess, and the patient's age. Although the vast majority of patients enjoy significant improvement and remission after proper medical care, health care providers should be aware of variability in the individual response to hyperthyroidism and individual sensitivity to thyroid hormone fluctuations generally. Graves' disease patients can also undergo periods of hypothyroidism, due to the challenges of finding the right dosage of thyroid hormone suppression and/or supplementation. The body's need for thyroid hormone can also change over time, such as in the first months after radioactive iodine treatment (RAI). Thyroid autoimmune diseases can also be volatile: hyperthyroidism can interchange with hypothyroidism and euthyroidism.
Antithyroid autoantibodies (or simply antithyroid antibodies) are autoantibodies targeted against one or more components on the thyroid. The most clinically relevant anti-thyroid autoantibodies are anti-thyroid peroxidase antibodies (anti-TPO antibodies, TPOAb), thyrotropin receptor antibodies (TRAb) and thyroglobulin antibodies (TgAb). TRAb's are subdivided into activating, blocking and neutral antibodies, depending on their effect on the TSH receptor. Anti-sodium/iodide (Anti–Na+/I−) symporter antibodies are a more recent discovery and their clinical relevance is still unknown. Graves' disease and Hashimoto's thyroiditis are commonly associated with the presence of anti-thyroid autoantibodies. Although there is overlap, anti-TPO antibodies are most commonly associated with Hashimoto's thyroiditis and activating TRAb's are most commonly associated with Graves' disease. Thyroid microsomal antibodies were a group of anti-thyroid antibodies; they were renamed after the identification of their target antigen (TPO).
References
- ↑ Nabhan ZM, Kreher NC, Eugster EA (April 2005). "Hashitoxicosis in children: clinical features and natural history". J. Pediatr. 146 (4): 533–6. doi:10.1016/j.jpeds.2004.10.070. PMID 15812459.
- ↑ Robins Basic Pathology