An abscess is a collection of pus that has built up within the tissue of the body. Signs and symptoms of abscesses include redness, pain, warmth, and swelling. The swelling may feel fluid-filled when pressed. The area of redness often extends beyond the swelling. Carbuncles and boils are types of abscess that often involve hair follicles, with carbuncles being larger. A cyst is related to an abscess, but it contains a material other than pus, and a cyst has a clearly defined wall.

Streptococcal pharyngitis, also known as streptococcal sore throat, is pharyngitis caused by Streptococcus pyogenes, a gram-positive, group A streptococcus. Common symptoms include fever, sore throat, red tonsils, and enlarged lymph nodes in the front of the neck. A headache and nausea or vomiting may also occur. Some develop a sandpaper-like rash which is known as scarlet fever. Symptoms typically begin one to three days after exposure and last seven to ten days.

Lemierre's syndrome is infectious thrombophlebitis of the internal jugular vein. It most often develops as a complication of a bacterial sore throat infection in young, otherwise healthy adults. The thrombophlebitis is a serious condition and may lead to further systemic complications such as bacteria in the blood or septic emboli.

Pharyngitis is inflammation of the back of the throat, known as the pharynx. It typically results in a sore throat and fever. Other symptoms may include a runny nose, cough, headache, difficulty swallowing, swollen lymph nodes, and a hoarse voice. Symptoms usually last 3–5 days, but can be longer depending on cause. Complications can include sinusitis and acute otitis media. Pharyngitis is a type of upper respiratory tract infection.

Cellulitis is usually a bacterial infection involving the inner layers of the skin. It specifically affects the dermis and subcutaneous fat. Signs and symptoms include an area of redness which increases in size over a few days. The borders of the area of redness are generally not sharp and the skin may be swollen. While the redness often turns white when pressure is applied, this is not always the case. The area of infection is usually painful. Lymphatic vessels may occasionally be involved, and the person may have a fever and feel tired.

Tonsillitis is inflammation of the tonsils in the upper part of the throat. It can be acute or chronic. Acute tonsillitis typically has a rapid onset. Symptoms may include sore throat, fever, enlargement of the tonsils, trouble swallowing, and enlarged lymph nodes around the neck. Complications include peritonsillar abscess (Quinsy).

Peritonsillar abscess (PTA), also known as quinsy, is an accumulation of pus due to an infection behind the tonsil. Symptoms include fever, throat pain, trouble opening the mouth, and a change to the voice. Pain is usually worse on one side. Complications may include blockage of the airway or aspiration pneumonitis.

Pyelonephritis is inflammation of the kidney, typically due to a bacterial infection. Symptoms most often include fever and flank tenderness. Other symptoms may include nausea, burning with urination, and frequent urination. Complications may include pus around the kidney, sepsis, or kidney failure.

Mastoiditis is the result of an infection that extends to the air cells of the skull behind the ear. Specifically, it is an inflammation of the mucosal lining of the mastoid antrum and mastoid air cell system inside the mastoid process. The mastoid process is the portion of the temporal bone of the skull that is behind the ear. The mastoid process contains open, air-containing spaces. Mastoiditis is usually caused by untreated acute otitis media and used to be a leading cause of child mortality. With the development of antibiotics, however, mastoiditis has become quite rare in developed countries where surgical treatment is now much less frequent and more conservative, unlike former times.

Ludwig's angina is a type of severe cellulitis involving the floor of the mouth and is often caused by bacterial sources. Early in the infection, the floor of the mouth raises due to swelling, leading to difficulty swallowing saliva. As a result, patients may present with drooling and difficulty speaking. As the condition worsens, the airway may be compromised and hardening of the spaces on both sides of the tongue may develop. Overall, this condition has a rapid onset over a few hours.

Lung abscess is a type of liquefactive necrosis of the lung tissue and formation of cavities containing necrotic debris or fluid caused by microbial infection.
Ampicillin/sulbactam is a fixed-dose combination medication of the common penicillin-derived antibiotic ampicillin and sulbactam, an inhibitor of bacterial beta-lactamase. Two different forms of the drug exist. The first, developed in 1987 and marketed in the United States under the brand name Unasyn, generic only outside the United States, is an intravenous antibiotic. The second, an oral form called sultamicillin, is marketed under the brand name Ampictam outside the United States, and generic only in the United States. Ampicillin/sulbactam is used to treat infections caused by bacteria resistant to beta-lactam antibiotics. Sulbactam blocks the enzyme which breaks down ampicillin and thereby allows ampicillin to attack and kill the bacteria.

Sultamicillin, sold under the brand name Unasyn among others, is an oral form of the penicillin antibiotic combination ampicillin/sulbactam. It is used for the treatment of bacterial infections of the upper and lower respiratory tract, the kidneys and urinary tract, skin and soft tissues, among other organs. It contains esterified ampicillin and sulbactam.
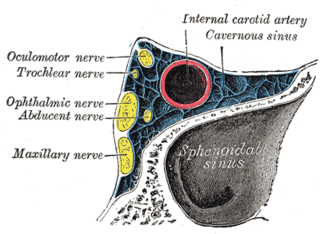
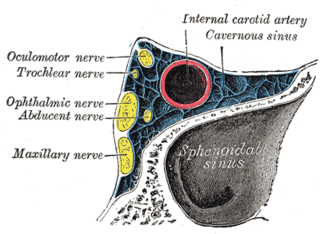
Cavernous sinus thrombosis (CST) is the formation of a blood clot within the cavernous sinus, a cavity at the base of the brain which drains deoxygenated blood from the brain back to the heart. This is a rare disorder and can be of two types–septic cavernous thrombosis and aseptic cavernous thrombosis. The most common form is septic cavernous sinus thrombosis. The cause is usually from a spreading infection in the nose, sinuses, ears, or teeth. Staphylococcus aureus and Streptococcus are often the associated bacteria.

Orbital cellulitis is inflammation of eye tissues behind the orbital septum. It is most commonly caused by an acute spread of infection into the eye socket from either the adjacent sinuses or through the blood. It may also occur after trauma. When it affects the rear of the eye, it is known as retro-orbital cellulitis.

Anorectal abscess is an abscess adjacent to the anus. Most cases of perianal abscesses are sporadic, though there are certain situations which elevate the risk for developing the disease, such as diabetes mellitus, Crohn's disease, chronic corticosteroid treatment and others. It arises as a complication of paraproctitis. Ischiorectal, inter- and intrasphincteric abscesses have been described.

A dental abscess is a localized collection of pus associated with a tooth. The most common type of dental abscess is a periapical abscess, and the second most common is a periodontal abscess. In a periapical abscess, usually the origin is a bacterial infection that has accumulated in the soft, often dead, pulp of the tooth. This can be caused by tooth decay, broken teeth or extensive periodontal disease. A failed root canal treatment may also create a similar abscess.
Pneumococcal infection is an infection caused by the bacterium Streptococcus pneumoniae.
Osteomyelitis of the jaws is osteomyelitis which occurs in the bones of the jaws. Historically, osteomyelitis of the jaws was a common complication of odontogenic infection. Before the antibiotic era, it was frequently a fatal condition.
There are many circumstances during dental treatment where antibiotics are prescribed by dentists to prevent further infection. The most common antibiotic prescribed by dental practitioners is penicillin in the form of amoxicillin, however many patients are hypersensitive to this particular antibiotic. Therefore, in the cases of allergies, erythromycin is used instead.