Related Research Articles
Ataxia is a neurological sign consisting of lack of voluntary coordination of muscle movements that can include gait abnormality, speech changes, and abnormalities in eye movements, that indicates dysfunction of parts of the nervous system that coordinate movement, such as the cerebellum.

A tremor is an involuntary, somewhat rhythmic muscle contraction and relaxation involving oscillations or twitching movements of one or more body parts. It is the most common of all involuntary movements and can affect the hands, arms, eyes, face, head, vocal folds, trunk, and legs. Most tremors occur in the hands. In some people, a tremor is a symptom of another neurological disorder.

Dystonia is a neurological hyperkinetic movement disorder in which sustained or repetitive muscle contractions occur involuntarily, resulting in twisting and repetitive movements or abnormal fixed postures. The movements may resemble a tremor. Dystonia is often intensified or exacerbated by physical activity, and symptoms may progress into adjacent muscles.

Multiple system atrophy (MSA) is a rare neurodegenerative disorder characterized by tremors, slow movement, muscle rigidity, postural instability, autonomic dysfunction and ataxia. This is caused by progressive degeneration of neurons in several parts of the brain including the basal ganglia, inferior olivary nucleus, and cerebellum.
Dysarthria is a speech sound disorder resulting from neurological injury of the motor component of the motor–speech system and is characterized by poor articulation of phonemes. It is a condition in which problems effectively occur with the muscles that help produce speech, often making it very difficult to pronounce words. It is unrelated to problems with understanding language, although a person can have both. Any of the speech subsystems can be affected, leading to impairments in intelligibility, audibility, naturalness, and efficiency of vocal communication. Dysarthria that has progressed to a total loss of speech is referred to as anarthria. The term dysarthria was formed from the Greek components dys- "dysfunctional, impaired" and arthr- "joint, vocal articulation".
Hyperkinesia refers to an increase in muscular activity that can result in excessive abnormal movements, excessive normal movements, or a combination of both. Hyperkinesia is a state of excessive restlessness which is featured in a large variety of disorders that affect the ability to control motor movement, such as Huntington's disease. It is the opposite of hypokinesia, which refers to decreased bodily movement, as commonly manifested in Parkinson's disease.

The inferior olivary nucleus (ION) is a structure found in the medulla oblongata underneath the superior olivary nucleus. In vertebrates, the ION is known to coordinate signals from the spinal cord to the cerebellum to regulate motor coordination and learning. These connections have been shown to be tightly associated, as degeneration of either the cerebellum or the ION results in degeneration of the other.
Astasis is a lack of motor coordination marked by an inability to stand, walk or even sit without assistance due to disruption of muscle coordination.
Hemiballismus or hemiballism is a basal ganglia syndrome resulting from damage to the subthalamic nucleus in the basal ganglia. It is a rare hyperkinetic movement disorder, that is characterized by pronounced involuntary limb movements on one side of the body and can cause significant disability. Rarely it affects both sides of the body. Symptoms can decrease during sleep.

Hypokinesia is one of the classifications of movement disorders, and refers to decreased bodily movement. Hypokinesia is characterized by a partial or complete loss of muscle movement due to a disruption in the basal ganglia. Hypokinesia is a symptom of Parkinson's disease shown as muscle rigidity and an inability to produce movement. It is also associated with mental health disorders and prolonged inactivity due to illness, amongst other diseases.
Dysmetria is a lack of coordination of movement typified by the undershoot or overshoot of intended position with the hand, arm, leg, or eye. It is a type of ataxia. It can also include an inability to judge distance or scale.

Spasmodic torticollis is an extremely painful chronic neurological movement disorder causing the neck to involuntarily turn to the left, right, upwards, and/or downwards. The condition is also referred to as "cervical dystonia". Both agonist and antagonist muscles contract simultaneously during dystonic movement. Causes of the disorder are predominantly idiopathic. A small number of patients develop the disorder as a result of another disorder or disease. Most patients first experience symptoms midlife. The most common treatment for spasmodic torticollis is the use of botulinum toxin type A.
Cerebellar ataxia is a form of ataxia originating in the cerebellum. Non-progressive congenital ataxia (NPCA) is a classical presentation of cerebral ataxias.
Intention tremor is a dyskinetic disorder characterized by a broad, coarse, and low-frequency tremor evident during deliberate and visually-guided movement. An intention tremor is usually perpendicular to the direction of movement. When experiencing an intention tremor, one often overshoots or undershoots one's target, a condition known as dysmetria. Intention tremor is the result of dysfunction of the cerebellum, particularly on the same side as the tremor in the lateral zone, which controls visually guided movements. Depending on the location of cerebellar damage, these tremors can be either unilateral or bilateral.

The signs and symptoms of multiple sclerosis (MS) encompass a wide range of neurological and physical manifestations, including vision problems, muscle weakness, coordination difficulties, and cognitive impairment, varying significantly in severity and progression among individuals.
Conjugate gaze palsies are neurological disorders affecting the ability to move both eyes in the same direction. These palsies can affect gaze in a horizontal, upward, or downward direction. These entities overlap with ophthalmoparesis and ophthalmoplegia.

The myoclonic triangle is an important feedback circuit of the brainstem and deep cerebellar nuclei which is responsible for modulating spinal cord motor activity.
Benedikt syndrome, also called Benedikt's syndrome or paramedian midbrain syndrome, is a rare type of posterior circulation stroke of the brain, with a range of neurological symptoms affecting the midbrain, cerebellum and other related structures.

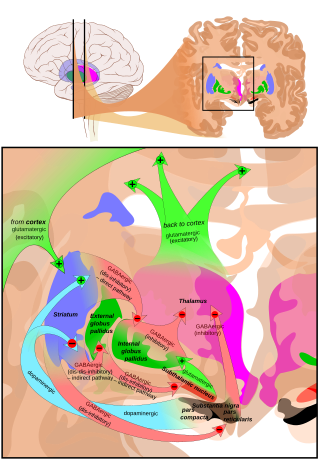
Basal ganglia disease is a group of physical problems that occur when the group of nuclei in the brain known as the basal ganglia fail to properly suppress unwanted movements or to properly prime upper motor neuron circuits to initiate motor function. Research indicates that increased output of the basal ganglia inhibits thalamocortical projection neurons. Proper activation or deactivation of these neurons is an integral component for proper movement. If something causes too much basal ganglia output, then the ventral anterior (VA) and ventral lateral (VL) thalamocortical projection neurons become too inhibited, and one cannot initiate voluntary movement. These disorders are known as hypokinetic disorders. However, a disorder leading to abnormally low output of the basal ganglia leads to reduced inhibition, and thus excitation, of the thalamocortical projection neurons which synapse onto the cortex. This situation leads to an inability to suppress unwanted movements. These disorders are known as hyperkinetic disorders.
Ataxic cerebral palsy is clinically in approximately 5–10% of all cases of cerebral palsy, making it the least frequent form of cerebral palsy diagnosed. Ataxic cerebral palsy is caused by damage to cerebellar structures, differentiating it from the other two forms of cerebral palsy, which are spastic cerebral palsy and dyskinetic cerebral palsy.
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 Puschmann, A; Wszolek, ZK (2011). "Diagnosis and Treatment of Common Forms of Tremor" (PDF). Seminars in Neurology. 31 (1): 65–77. doi:10.1055/s-0031-1271312. PMC 3907068 . PMID 21321834.
- 1 2 3 4 Menon, B; Sasikala, P; Agrawal, A (2014). "Giant Middle Fossa Epidermoid Presenting as Holmes' tremor Syndrome". Journal of Movement Disorders. 7 (1): 22–24. doi:10.14802/jmd.14005. PMC 4051724 . PMID 24926407.
- 1 2 3 4 Buijink, A; Contarino, M; Koelman, J; Speelman, J; van Rootselaar, A (2012). "How to Tackle Tremor – Systematic Review of the Literature and Diagnostic Work-Up". Frontiers in Neurology. 3 (146): 146. doi: 10.3389/fneur.2012.00146 . PMC 3478569 . PMID 23109928.