Health equity arises from access to the social determinants of health, specifically from wealth, power and prestige. Individuals who have consistently been deprived of these three determinants are significantly disadvantaged from health inequities, and face worse health outcomes than those who are able to access certain resources. It is not equity to simply provide every individual with the same resources; that would be equality. In order to achieve health equity, resources must be allocated based on an individual need-based principle.

The Johns Hopkins Bloomberg School of Public Health is the public health graduate school of Johns Hopkins University, a private research university in Baltimore, Maryland. As the second independent, degree-granting institution for research in epidemiology and training in public health, and the largest public health training facility in the United States.

In medicine, rural health or rural medicine is the interdisciplinary study of health and health care delivery in rural environments. The concept of rural health incorporates many fields, including wilderness medicine, geography, midwifery, nursing, sociology, economics, and telehealth or telemedicine.
Race and health refers to how being identified with a specific race influences health. Race is a complex concept that has changed across chronological eras and depends on both self-identification and social recognition. In the study of race and health, scientists organize people in racial categories depending on different factors such as: phenotype, ancestry, social identity, genetic makeup and lived experience. "Race" and ethnicity often remain undifferentiated in health research.
The Johns Hopkins University School of Nursing (JHUSON) is the nursing school of Johns Hopkins University in Baltimore, Maryland. Established in 1889, it is one of the nation's oldest schools for nursing education. It is continuously rated as the top nursing program in the US per U.S. News & World Report.
Residential segregation is the physical separation of two or more groups into different neighborhoods—a form of segregation that "sorts population groups into various neighborhood contexts and shapes the living environment at the neighborhood level". While it has traditionally been associated with racial segregation, it generally refers to the separation of populations based on some criteria.

The Tulane School of Public Health and Tropical Medicine is part of Tulane University, located in New Orleans, in the U.S. state of Louisiana.
Health Disparities Centers are institutions in the United States that cover a broad range of needs and focus areas to decrease currently disproportionate illness and disease rates that lead to health disparities. They also promote the engagement, empowerment and recruitment of underrepresented populations in health professions. Many programs devote significant resources to developing cultural competency training to promote the delivery of culturally sensitive healthcare by faculty and staff, as well as current and future healthcare providers. These services are usually tailored to meeting specific goals or missions of the individual components common in most of the operating Health Disparities Centers.
Lisa A. Cooper is an American internal medicine and public health physician who is the Bloomberg Distinguished Professor of Equity in Health and Healthcare at Johns Hopkins University, jointly appointed in the Johns Hopkins School of Medicine, Johns Hopkins School of Nursing and in the departments of Health, Behavior and Society, Health Policy and Management; Epidemiology; and International Health in the Johns Hopkins Bloomberg School of Public Health. She is the James F. Fries Professor of Medicine in the Division of General Internal Medicine, Director of the Johns Hopkins Center for Health Equity, and Director of the Johns Hopkins Urban Health Institute. Cooper is also a Gilman Scholar and a core faculty member in the Welch Center for Prevention, Epidemiology, and Clinical Research. She is internationally recognized for her research on the impact of race, ethnicity and gender on the patient-physician relationship and subsequent health disparities. She is a member of the President’s Council of Advisors on Science and Technology (PCAST). In 2007, she received a MacArthur Fellowship.
The National Institute on Minority Health and Health Disparities (NIMHD) is an American government health institute. It is part of the National Institutes of Health (NIH). The stated mission of the NIMHD is to "lead scientific research to improve minority health and eliminate health disparities."
Research shows many health disparities among different racial and ethnic groups in the United States. Different outcomes in mental and physical health exist between all U.S. Census-recognized racial groups, but these differences stem from different historical and current factors, including genetics, socioeconomic factors, and racism. Research has demonstrated that numerous health care professionals show implicit bias in the way that they treat patients. Certain diseases have a higher prevalence among specific racial groups, and life expectancy also varies across groups.
Structural inequality occurs when the fabric of organizations, institutions, governments or social networks contains an embedded cultural, linguistic, economic, religious/belief, physical or identity based bias which provides advantages for some members and marginalizes or produces disadvantages for other members. This can involve, personal agency, freedom of expression, property rights, freedom of association, religious freedom,social status, or unequal access to health care, housing, education, physical, cultural, social, religious or political belief, financial resources or other social opportunities. Structural inequality is believed to be an embedded part of all known cultural groups. The global history of slavery, serfdom, indentured servitude and other forms of coerced cultural or government mandated labour or economic exploitation that marginalizes individuals and the subsequent suppression of human rights are key factors defining structural inequality.
This article summarizes healthcare in Texas. In 2022, the United Healthcare Foundation ranked Texas as the 38th healthiest state in the United States. Obesity, excessive drinking, maternal mortality, infant mortality, vaccinations, mental health, and limited access to healthcare are among the major public health issues facing Texas.

Cultural competence in healthcare refers to the ability for healthcare professionals to demonstrate cultural competence toward patients with diverse values, beliefs, and feelings. This process includes consideration of the individual social, cultural, and psychological needs of patients for effective cross-cultural communication with their health care providers. The goal of cultural competence in health care is to reduce health disparities and to provide optimal care to patients regardless of their race, gender, ethnic background, native languages spoken, and religious or cultural beliefs. Cultural competency training is important in health care fields where human interaction is common, including medicine, nursing, allied health, mental health, social work, pharmacy, oral health, and public health fields.
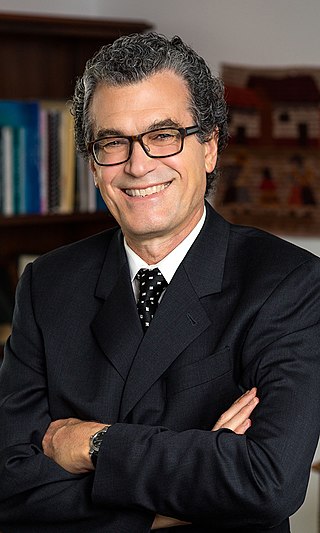
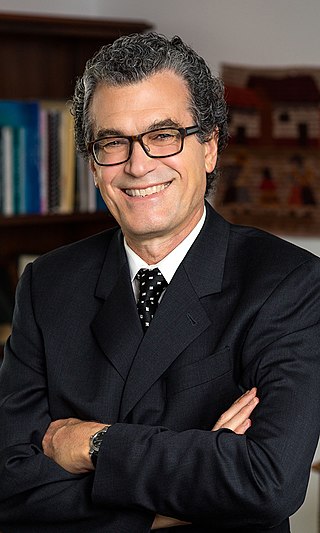
Thomas A. LaVeist is the dean and Weatherhead Presidential Chair at the School of Public Health and Tropical Medicine at Tulane University in New Orleans, Louisiana. He was previously the chairman of the Department of Health Policy and Management at the George Washington University, Milken Institute School of Public Health. He focuses mainly on the development of policy and interventions to address race disparities in the health field.
Mental health inequality refers to the differences in the quality, access, and health care different communities and populations receive for mental health services. Globally, the World Health Organization estimates that 350 million people are affected with depressive disorders. Mental health can be defined as an individual's well-being and/or the absence of clinically defined mental illness. Inequalities that can occur in mental healthcare may include mental health status, access to and quality of care, and mental health outcomes, which may differ across populations of different race, ethnicity, sexual orientation, sex, gender, socioeconomic statuses, education level, and geographic location. Social determinants of health, more specifically the social determinants of mental health, that can influence an individual's susceptibility to developing mental disorders and illnesses include, but are not limited to, economic status, education level, demographics, geographic location and genetics.

Rachel Renee Hardeman is an American public health academic who is associate professor of Division of Health Policy and Management at the University of Minnesota School of Public Health. She holds the inaugural Blue Cross Endowed Professorship in Health and Racial Equity. Her research considers how racism impacts health outcomes, particularly for the maternal health of African-Americans.
Tonia C. Poteat is an American epidemiologist. She is an associate professor of Social Medicine at the University of North Carolina where she focuses on HIV, having previously worked at the Johns Hopkins Bloomberg School of Public Health.
Sarah Loeb Szanton is an American nurse practitioner who focuses on geriatric nursing research. As of 2021, she is the Dean of the Johns Hopkins School of Nursing.
The gap in socioeconomic status between racial groups in South Africa has been a key contributor to health disparities, with White South Africans, a minority group, having overall better health outcomes than majority Black South Africans. White South Africans, a minority group, have overall better access and health outcomes than other racial groups in South Africa. Black and Colored South Africans, have poorer overall health outcomes and are disproportionately unable to access the private healthcare system in South Africa.