Related Research Articles
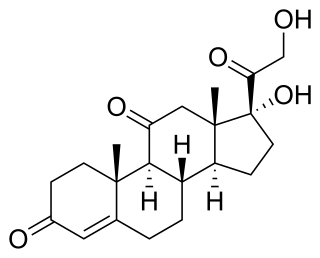
Cortisone is a pregnene (21-carbon) steroid hormone. It is a naturally-occurring corticosteroid metabolite that is also used as a pharmaceutical prodrug. Cortisol is converted by the action of the enzyme corticosteroid 11-beta-dehydrogenase isozyme 2 into the inactive metabolite cortisone, particularly in the kidneys. This is done by oxidizing the alcohol group at carbon 11. Cortisone is converted back to the active steroid cortisol by stereospecific hydrogenation at carbon 11 by the enzyme 11β-Hydroxysteroid dehydrogenase type 1, particularly in the liver.
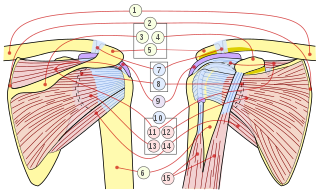
The rotator cuff is a group of muscles and their tendons that act to stabilize the human shoulder and allow for its extensive range of motion. Of the seven scapulohumeral muscles, four make up the rotator cuff. The four muscles are:

Shoulder problems including pain, are one of the more common reasons for physician visits for musculoskeletal symptoms. The shoulder is the most movable joint in the body. However, it is an unstable joint because of the range of motion allowed. This instability increases the likelihood of joint injury, often leading to a degenerative process in which tissues break down and no longer function well.

Bowel obstruction, also known as intestinal obstruction, is a mechanical or functional obstruction of the intestines which prevents the normal movement of the products of digestion. Either the small bowel or large bowel may be affected. Signs and symptoms include abdominal pain, vomiting, bloating and not passing gas. Mechanical obstruction is the cause of about 5 to 15% of cases of severe abdominal pain of sudden onset requiring admission to hospital.

Adhesive capsulitis (AC), also known as frozen shoulder, is a condition associated with shoulder pain and stiffness. It is a common shoulder ailment that is marked by pain and a loss of range of motion, particularly in external rotation. There is a loss of the ability to move the shoulder, both voluntarily and by others, in multiple directions. The shoulder itself, however, does not generally hurt significantly when touched. Muscle loss around the shoulder may also occur. Onset is gradual over weeks to months. Complications can include fracture of the humerus or biceps tendon rupture.

Nerve block or regional nerve blockade is any deliberate interruption of signals traveling along a nerve, often for the purpose of pain relief. Local anesthetic nerve block is a short-term block, usually lasting hours or days, involving the injection of an anesthetic, a corticosteroid, and other agents onto or near a nerve. Neurolytic block, the deliberate temporary degeneration of nerve fibers through the application of chemicals, heat, or freezing, produces a block that may persist for weeks, months, or indefinitely. Neurectomy, the cutting through or removal of a nerve or a section of a nerve, usually produces a permanent block. Because neurectomy of a sensory nerve is often followed, months later, by the emergence of new, more intense pain, sensory nerve neurectomy is rarely performed.

An arthrogram is a series of images of a joint after injection of a contrast medium, usually done by fluoroscopy or MRI. The injection is normally done under a local anesthetic such as Novocain or lidocaine. The radiologist or radiographer performs the study using fluoroscopy or x-ray to guide the placement of the needle into the joint and then injects around 10 ml of contrast based on age. There is some burning pain from the anesthetic and a painful bubbling feeling in the joint after the contrast is injected. This only lasts 20 – 30 hours until the Contrast is absorbed. During this time, while it is allowed, it is painful to use the limb for around 10 hours. After that the radiologist can more clearly see what is going on under your skin and can get results out within 24 to 48 hours.

An enthesopathy refers to a disorder involving the attachment of a tendon or ligament to a bone. This site of attachment is known as the enthesis . If the condition is known to be inflammatory, it can more precisely be called an enthesitis.

The shoulder joint is structurally classified as a synovial ball-and-socket joint and functionally as a diarthrosis and multiaxial joint. It involves an articulation between the glenoid fossa of the scapula and the head of the humerus. Due to the very loose joint capsule, it gives a limited interface of the humerus and scapula, it is the most mobile joint of the human body.
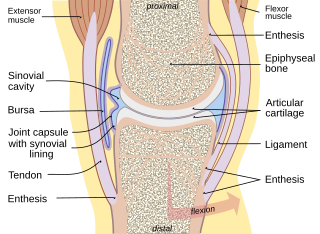
In anatomy, a joint capsule or articular capsule is an envelope surrounding a synovial joint. Each joint capsule has two parts: an outer fibrous layer or membrane, and an inner synovial layer or membrane.

The coracohumeral ligament is a broad ligament of the shoulder. It attaches to the coracoid process at one end, and to the greater and lesser tubercles of the humerus at the other. It strengthens the upper part of the joint capsule of the shoulder joint.

Adhesions are fibrous bands that form between tissues and organs, often as a result of injury during surgery. They may be thought of as internal scar tissue that connects tissues not normally connected.

Subacromial bursitis is a condition caused by inflammation of the bursa that separates the superior surface of the supraspinatus tendon from the overlying coraco-acromial ligament, acromion, and coracoid and from the deep surface of the deltoid muscle. The subacromial bursa helps the motion of the supraspinatus tendon of the rotator cuff in activities such as overhead work.

Degloving occurs when skin and the fat below it, the subcutaneous tissue, are torn away from the underlying anatomical structures they are normally attached to. Normally the subcutaneous tissue layer is attached to the fibrous layer that covers muscles known as deep fascia.
Arthrofibrosis has been described in most joints like knee, hip, ankle, foot joints, shoulder, elbow, wrist, hand joints as well as spinal vertebrae. It can occur after injury or surgery or may arise without an obvious cause. There is excessive scar tissue formation within the joint and/or surrounding soft tissues leading to painful restriction of joint motion that persists despite physical therapy and rehabilitation. The scar tissue may be located inside the knee joint or may involve the soft tissue structures around the knee joint, or both locations.

The capsule of the glenohumeral (shoulder) joint is the articular capsule of the shoulder. It completely surrounds the joint. It is attached above to the circumference of the glenoid cavity beyond the glenoidal labrum, and below to the anatomical neck of the humerus, approaching nearer to the articular cartilage above than in the rest of its extent.
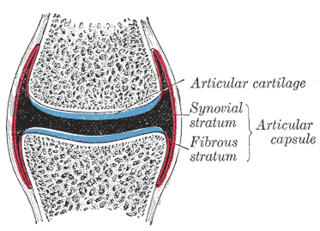
In anatomy, capsulitis is inflammation of a capsule.

Facet joint injections are used to alleviate symptoms of Facet syndrome. The procedure is an outpatient surgery, so that the patient can go home on the same day. It usually takes 10–20 minutes, but may take up to 30 minutes if the patient needs an IV for relaxation. Facet joint injections came into use from 1963, when Hirsch injected a hypertonic solution of saline into facet joints. He found that this solution relieved lower back pain in the sacroiliac and gluteal regions of the spine. In 1979 fluoroscopy was used for guidance of the needle into the facet joints with steroids and local anesthetics.

Facet syndrome is a syndrome in which the facet joints cause painful symptoms. In conjunction with degenerative disc disease, a distinct but functionally related condition, facet arthropathy is believed to be one of the most common causes of lower back pain.

A proximal humerus fracture is a break of the upper part of the bone of the arm (humerus). Symptoms include pain, swelling, and a decreased ability to move the shoulder. Complications may include axillary nerve or axillary artery injury.
References
- ↑ "Shoulder Hydrodilatation | Advanced Orthopaedics & Sports Medicine, Orthopaedic Specialists, Cypress, Houston, TX". www.advancedosm.com. Retrieved 2024-12-24.
- ↑ Tveitå EK, Tariq R, Sesseng S, Juel NG, Bautz-Holter E (2008). "Hydrodilatation, corticosteroids and adhesive capsulitis: a randomized controlled trial". BMC Musculoskelet Disord. 9: 53. doi: 10.1186/1471-2474-9-53 . PMC 2374785 . PMID 18423042.
{{cite journal}}: CS1 maint: multiple names: authors list (link)