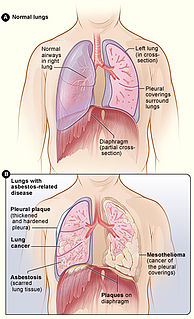
Asbestosis is long-term inflammation and scarring of the lungs due to asbestos fibers. Symptoms may include shortness of breath, cough, wheezing, and chest tightness. Complications may include lung cancer, mesothelioma, and pulmonary heart disease.

Silicosis is a form of occupational lung disease caused by inhalation of crystalline silica dust. It is marked by inflammation and scarring in the form of nodular lesions in the upper lobes of the lungs. It is a type of pneumoconiosis. Silicosis is characterized by shortness of breath, cough, fever, and cyanosis. It may often be misdiagnosed as pulmonary edema, pneumonia, or tuberculosis.
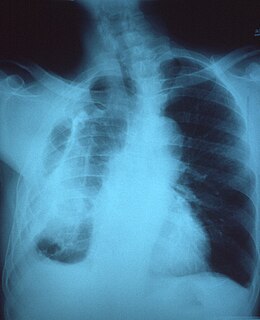
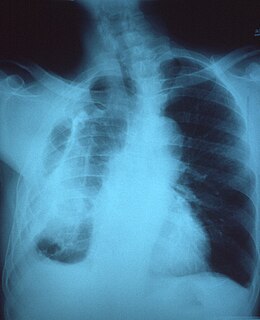
Radiology (X-rays) is used in the diagnosis of tuberculosis. Abnormalities on chest radiographs may be suggestive of, but are never diagnostic of TB, but can be used to rule out pulmonary TB.

Interstitial lung disease (ILD), or diffuse parenchymal lung disease (DPLD), is a group of respiratory diseases affecting the interstitium (the tissue and space around the alveoli of the lungs. It concerns alveolar epithelium, pulmonary capillary endothelium, basement membrane, and perivascular and perilymphatic tissues. It may occur when an injury to the lungs triggers an abnormal healing response. Ordinarily, the body generates just the right amount of tissue to repair damage, but in interstitial lung disease, the repair process is disrupted, and the tissue around the air sacs becomes scarred and thickened. This makes it more difficult for oxygen to pass into the bloodstream. The disease presents itself with the following symptoms: shortness of breath, nonproductive coughing, fatigue, and weight loss, which tend to develop slowly, over several months. The average rate of survival for someone with this disease is between three and five years. The term ILD is used to distinguish these diseases from obstructive airways diseases.

A chest radiograph, called a chest X-ray (CXR), or chest film, is a projection radiograph of the chest used to diagnose conditions affecting the chest, its contents, and nearby structures. Chest radiographs are the most common film taken in medicine.

Coal workers' pneumoconiosis (CWP), also known as black lung disease or black lung, is caused by long-term exposure to coal dust. It is common in coal miners and others who work with coal. It is similar to both silicosis from inhaling silica dust and asbestosis from inhaling asbestos dust. Inhaled coal dust progressively builds up in the lungs and leads to inflammation, fibrosis, and in worse cases, necrosis.
Progressive massive fibrosis (PMF), characterized by the development of large conglomerate masses of dense fibrosis, can complicate silicosis and coal worker's pneumoconiosis. Conglomerate masses may also occur in other pneumoconioses, such as talcosis, berylliosis (CBD), kaolin pneumoconiosis, and pneumoconiosis from carbon compounds, such as carbon black, graphite, and oil shale. Conglomerate masses can also develop in sarcoidosis, but usually near the hilae and with surrounding paracicatricial emphysema.
Kerley lines are a sign seen on chest radiographs with interstitial pulmonary edema. They are thin linear pulmonary opacities caused by fluid or cellular infiltration into the interstitium of the lungs. They are named after Irish neurologist and radiologist Peter Kerley.
Baritosis is a benign type of pneumoconiosis, which is caused by long-term exposure to barium dust.

Usual interstitial pneumonia (UIP) is a form of lung disease characterized by progressive scarring of both lungs. The scarring (fibrosis) involves the supporting framework (interstitium) of the lung. UIP is thus classified as a form of interstitial lung disease.

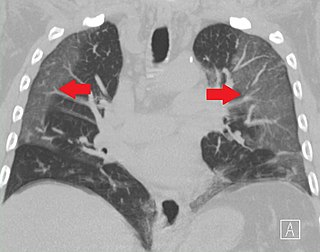
High-resolution computed tomography (HRCT) is a type of computed tomography (CT) with specific techniques to enhance image resolution. It is used in the diagnosis of various health problems, though most commonly for lung disease, by assessing the lung parenchyma.
Malignant pleural effusion is a condition in which cancer causes an abnormal amount of fluid to collect between the thin layers of tissue (pleura) lining the outside of the lung and the wall of the chest cavity. Lung cancer and breast cancer account for about 50-65% of malignant pleural effusions. Other common causes include pleural mesothelioma and lymphoma.

Peribronchial cuffing, also referred to as peribronchial thickening or bronchial wall thickening, is a radiologic sign which occurs when excess fluid or mucus buildup in the small airway passages of the lung causes localized patches of atelectasis. This causes the area around the bronchus to appear more prominent on an X-ray. It has also been described as donut sign, considering the edge is thicker, and the center contains air.
Pleural disease occurs in the pleural space, which is the thin fluid-filled area in between the two pulmonary pleurae in the human body. There are several disorders and complications that can occur within the pleural area, and the surrounding tissues in the lung.
Fibrothorax is a medical condition characterised by severe scarring (fibrosis) and fusion of the layers of the pleural space surrounding the lungs resulting in decreased movement of the lung and ribcage. The main symptom of fibrothorax is shortness of breath. There also may be recurrent fluid collections surrounding the lungs. Fibrothorax may occur as a complication of many diseases, including infection of the pleural space known as an empyema or bleeding into the pleural space known as a haemothorax.
A "B" reader is a physician certified by the National Institute for Occupational Safety and Health (NIOSH) as demonstrating proficiency in classifying radiographs of the pneumoconioses.
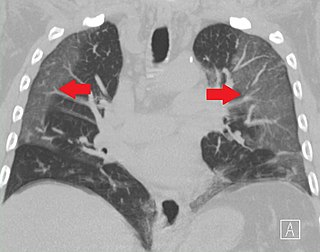
Ground-glass opacity (GGO) is a finding seen on chest x-ray (radiograph) or computed tomography (CT) imaging of the lungs. It is typically defined as an area of hazy opacification (x-ray) or increased attenuation (CT) due to air displacement by fluid, airway collapse, fibrosis, or a neoplastic process. When a substance other than air fills an area of the lung it increases that area's density. On both x-ray and CT, this appears more grey or hazy as opposed to the normally dark-appearing lungs. Although it can sometimes be seen in normal lungs, common pathologic causes include infections, interstitial lung disease, and pulmonary edema.
Tumor-like disorders of the lung pleura are a group of conditions that on initial radiological studies might be confused with malignant lesions. Radiologists must be aware of these conditions in order to avoid misdiagnosing patients. Examples of such lesions are: pleural plaques, thoracic splenosis, catamenial pneumothorax, pleural pseudotumor, diffuse pleural thickening, diffuse pulmonary lymphangiomatosis and Erdheim–Chester disease.
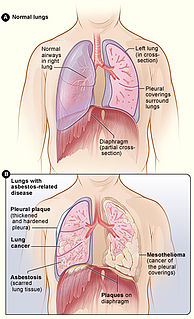
Asbestos-related diseases are disorders of the lung and pleura caused by the inhalation of asbestos fibres. Asbestos-related diseases include non-malignant disorders such as asbestosis, diffuse pleural thickening, pleural plaques, pleural effusion, rounded atelectasis and malignancies such as lung cancer and malignant mesothelioma.
Indium lung is a rare occupational lung disease caused by exposure to respirable indium in the form of indium tin oxide. It is classified as an interstitial lung disease.