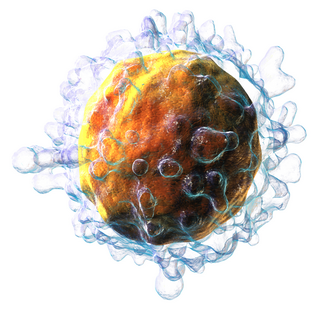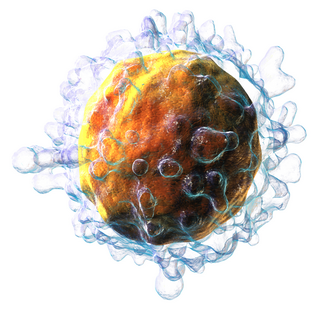
T cells are one of the important types of white blood cells of the immune system and play a central role in the adaptive immune response. T cells can be distinguished from other lymphocytes by the presence of a T-cell receptor (TCR) on their cell surface.
Immunotherapy or biological therapy is the treatment of disease by activating or suppressing the immune system. Immunotherapies designed to elicit or amplify an immune response are classified as activation immunotherapies, while immunotherapies that reduce or suppress are classified as suppression immunotherapies. Immunotherapy is under preliminary research for its potential to treat various forms of cancer.
Anergy, within the realm of immunology, characterizes the absence of a response from the body's defense mechanisms when confronted with foreign substances. This phenomenon involves the direct induction of peripheral lymphocyte tolerance. When an individual is in a state of anergy, it signifies that their immune system is incapable of mounting a typical response against a specific antigen, typically a self-antigen. The term anergy specifically refers to lymphocytes that exhibit an inability to react to their designated antigen. Notably, anergy constitutes one of the essential processes fostering tolerance within the immune system, alongside clonal deletion and immunoregulation. These processes collectively act to modify the immune response, preventing the inadvertent self-destruction that could result from an overactive immune system.
The regulatory T cells (Tregs or Treg cells), formerly known as suppressor T cells, are a subpopulation of T cells that modulate the immune system, maintain tolerance to self-antigens, and prevent autoimmune disease. Treg cells are immunosuppressive and generally suppress or downregulate induction and proliferation of effector T cells. Treg cells express the biomarkers CD4, FOXP3, and CD25 and are thought to be derived from the same lineage as naïve CD4+ cells. Because effector T cells also express CD4 and CD25, Treg cells are very difficult to effectively discern from effector CD4+, making them difficult to study. Research has found that the cytokine transforming growth factor beta (TGF-β) is essential for Treg cells to differentiate from naïve CD4+ cells and is important in maintaining Treg cell homeostasis.
Alloimmunity is an immune response to nonself antigens from members of the same species, which are called alloantigens or isoantigens. Two major types of alloantigens are blood group antigens and histocompatibility antigens. In alloimmunity, the body creates antibodies against the alloantigens, attacking transfused blood, allotransplanted tissue, and even the fetus in some cases. Alloimmune (isoimmune) response results in graft rejection, which is manifested as deterioration or complete loss of graft function. In contrast, autoimmunity is an immune response to the self's own antigens. Alloimmunization (isoimmunization) is the process of becoming alloimmune, that is, developing the relevant antibodies for the first time.

FOXP3, also known as scurfin, is a protein involved in immune system responses. A member of the FOX protein family, FOXP3 appears to function as a master regulator of the regulatory pathway in the development and function of regulatory T cells. Regulatory T cells generally turn the immune response down. In cancer, an excess of regulatory T cell activity can prevent the immune system from destroying cancer cells. In autoimmune disease, a deficiency of regulatory T cell activity can allow other autoimmune cells to attack the body's own tissues.

Heligmosomoides polygyrus, previously named Nematospiroides dubius, is a naturally occurring intestinal roundworm of rodents. It belongs to the family Trychostrongylidae, and male and female worms are morphologically distinguishable. The parasite has a direct lifecycle, with its larval form being the infective stage. H. polygyrus has the ability to establish chronic infections in rodents and alter host immune responses. This nematode is widely used as a gastrointestinal parasitic model in immunological, pharmacological, and toxicological studies.
Immune tolerance, also known as immunological tolerance or immunotolerance, refers to the immune system's state of unresponsiveness to substances or tissues that would otherwise trigger an immune response. It arises from prior exposure to a specific antigen and contrasts the immune system's conventional role in eliminating foreign antigens. Depending on the site of induction, tolerance is categorized as either central tolerance, occurring in the thymus and bone marrow, or peripheral tolerance, taking place in other tissues and lymph nodes. Although the mechanisms establishing central and peripheral tolerance differ, their outcomes are analogous, ensuring immune system modulation.
Certain sites of the mammalian body have immune privilege, meaning they are able to tolerate the introduction of antigens without eliciting an inflammatory immune response. Tissue grafts are normally recognised as foreign antigens by the body and attacked by the immune system. However, in immune privileged sites, tissue grafts can survive for extended periods of time without rejection occurring. Immunologically privileged sites include:
In immunology, peripheral tolerance is the second branch of immunological tolerance, after central tolerance. It takes place in the immune periphery. Its main purpose is to ensure that self-reactive T and B cells which escaped central tolerance do not cause autoimmune disease. Peripheral tolerance can also serve a purpose in preventing an immune response to harmless food antigens and allergens.

Lymphocyte-activation gene 3, also known as LAG-3, is a protein which in humans is encoded by the LAG3 gene. LAG3, which was discovered in 1990 and was designated CD223 after the Seventh Human Leucocyte Differentiation Antigen Workshop in 2000, is a cell surface molecule with diverse biological effects on T cell function but overall has an immune inhibitory effect. It is an immune checkpoint receptor and as such is the target of various drug development programs by pharmaceutical companies seeking to develop new treatments for cancer and autoimmune disorders. In soluble form it is also being developed as a cancer drug in its own right.

The Interleukin-2 receptor alpha chain is a protein involved in the assembly of the high-affinity Interleukin-2 receptor, consisting of alpha (IL2RA), beta (IL2RB) and the common gamma chain (IL2RG). As the name indicates, this receptor interacts with Interleukin-2, a pleiotropic cytokine which plays an important role in immune homeostasis.
T helper 3 cells (Th3) are a subset of T lymphocytes with immunoregulary and immunosuppressive functions, that can be induced by administration of foreign oral antigen. Th3 cells act mainly through the secretion of anti-inflammatory cytokine transforming growth factor beta (TGF-β). Th3 have been described both in mice and human as CD4+FOXP3− regulatory T cells. Th3 cells were first described in research focusing on oral tolerance in the experimental autoimmune encephalitis (EAE) mouse model and later described as CD4+CD25−FOXP3−LAP+ cells, that can be induced in the gut by oral antigen through T cell receptor (TCR) signalling.
Short Course Immune Induction Therapy or SCIIT, is a therapeutic strategy employing rapid, specific, short term-modulation of the immune system using a therapeutic agent to induce T-cell non-responsiveness, also known as operational tolerance. As an alternative strategy to immunosuppression and antigen-specific tolerance inducing therapies, the primary goal of SCIIT is to re-establish or induce peripheral immune tolerance in the context of autoimmune disease and transplant rejection through the use of biological agents. In recent years, SCIIT has received increasing attention in clinical and research settings as an alternative to immunosuppressive drugs currently used in the clinic, drugs which put the patients at risk of developing infection, cancer, and cardiovascular disease.

Dame Fiona Magaret Powrie is currently the head of the Kennedy Institute of Rheumatology at the University of Oxford. Formerly she was the inaugural Sidney Truelove Professor of Gastroenterology at the University of Oxford. She is also head of the Experimental Medicine Division of the Nuffield Department of Clinical Medicine.
Regulatory B cells (Bregs or Breg cells) represent a small population of B cells that participates in immunomodulation and in the suppression of immune responses. The population of Bregs can be further separated into different human or murine subsets such as B10 cells, marginal zone B cells, Br1 cells, GrB+B cells, CD9+ B cells, and even some plasmablasts or plasma cells. Bregs regulate the immune system by different mechanisms. One of the main mechanisms is the production of anti-inflammatory cytokines such as interleukin 10 (IL-10), IL-35, or transforming growth factor beta (TGF-β). Another known mechanism is the production of cytotoxic Granzyme B. Bregs also express various inhibitory surface markers such as programmed death-ligand 1 (PD-L1), CD39, CD73, and aryl hydrocarbon receptor. The regulatory effects of Bregs were described in various models of inflammation, autoimmune diseases, transplantation reactions, and in anti-tumor immunity.
Regulatory macrophages (Mregs) represent a subset of anti-inflammatory macrophages. In general, macrophages are a very dynamic and plastic cell type and can be divided into two main groups: classically activated macrophages (M1) and alternatively activated macrophages (M2). M2 group can further be divided into sub-groups M2a, M2b, M2c, and M2d. Typically the M2 cells have anti-inflammatory and regulatory properties and produce many different anti-inflammatory cytokines such as IL-4, IL-33, IL-10, IL-1RA, and TGF-β. M2 cells can also secrete angiogenic and chemotactic factors. These cells can be distinguished based on the different expression levels of various surface proteins and the secretion of different effector molecules.
Tolerogenic therapy aims to induce immune tolerance where there is pathological or undesirable activation of the normal immune response. This can occur, for example, when an allogeneic transplantation patient develops an immune reaction to donor antigens, or when the body responds inappropriately to self antigens implicated in autoimmune diseases. It must provide absence of specific antibodies for exactly that antigenes.
Type 1 regulatory cells or Tr1 (TR1) cells are a class of regulatory T cells participating in peripheral immunity as a subsets of CD4+ T cells. Tr1 cells regulate tolerance towards antigens of any origin. Tr1 cells are self or non-self antigen specific and their key role is to induce and maintain peripheral tolerance and suppress tissue inflammation in autoimmunity and graft vs. host disease.
Tolerogenic dendritic cells are heterogenous pool of dendritic cells with immuno-suppressive properties, priming immune system into tolerogenic state against various antigens. These tolerogenic effects are mostly mediated through regulation of T cells such as inducing T cell anergy, T cell apoptosis and induction of Tregs. Tol-DCs also affect local micro-environment toward tolerogenic state by producing anti-inflammatory cytokines.