Mechanisms
Placental mechanisms
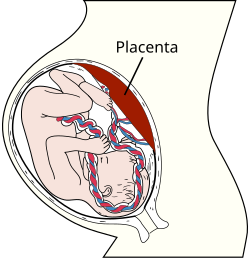
The placenta functions as an immunological barrier between the mother and the fetus, creating an immunologically privileged site. For this purpose, it uses several mechanisms:
- It secretes neurokinin B containing phosphocholine molecules. This is the same mechanism used by parasitic nematodes to avoid detection by the immune system of their host. [3]
- Also, there is the presence of small lymphocytic suppressor cells in the fetus that inhibit maternal cytotoxic T cells by inhibiting the response to interleukin 2. [2]
- The placental trophoblast cells do not express the classical MHC class I isotypes HLA-A and HLA-B, unlike most other cells in the body, and this absence is assumed to prevent destruction by maternal cytotoxic T cells, which otherwise would recognize the fetal HLA-A and HLA-B molecules as foreign. On the other hand, they do express the atypical MHC class I isotypes HLA-E and HLA-G, which is assumed to prevent destruction by maternal natural killer cells, which otherwise destroy cells that do not express any MHC class I. [4] However, trophoblast cells do express the rather typical HLA-C. [4]
- It forms a syncytium without any extracellular spaces between cells in order to limit the exchange of migratory immune cells between the developing embryo and the body of the mother (something an epithelium will not do sufficiently, as certain blood cells are specialized to be able to insert themselves between adjacent epithelial cells). The fusion of the cells is apparently caused by viral fusion proteins from endosymbiotic endogenous retrovirus. [5] An immunoevasive action was the initial normal behavior of the viral protein, in order to avail for the virus to spread to other cells by simply merging them with the infected one. It is believed that the ancestors of modern viviparous mammals evolved after an infection by this virus, enabling the fetus to better resist the immune system of the mother. [6]
Still, the placenta does allow maternal immunoglobulin G (IgG) to pass to the fetus to protect it against infections. However, these antibodies do not target fetal cells, unless any fetal material has escaped across the placenta where it can come in contact with maternal B cells and make those B cells start to produce antibodies against fetal targets. The mother does produce antibodies against foreign ABO blood types, where the fetal blood cells are possible targets, but these preformed antibodies are usually of the immunoglobulin M type, [7] and therefore usually do not cross the placenta. Still, rarely, ABO incompatibility can give rise to IgG antibodies that cross the placenta, and are caused by sensitization of mothers (usually of blood type O) to antigens in foods or bacteria that are homologous to A and B antigens. [8]
Other mechanisms
Still, the placental barrier is not the sole means to evade the immune system, as foreign fetal cells also persist in the maternal circulation, on the other side of the placental barrier. [9]
The placenta does not block maternal IgG antibodies, which thereby may pass through the human placenta, providing immune protection to the fetus against infectious diseases.
One model for the induction of tolerance during the very early stages of pregnancy is the eutherian fetoembryonic defense system (eu-FEDS) hypothesis. [10] The basic premise of the eu-FEDS hypothesis is that both soluble and cell surface associated glycoproteins, present in the reproductive system and expressed on gametes, suppress any potential immune responses, and inhibit rejection of the fetus. [10] The eu-FEDS model further suggests that specific carbohydrate sequences (oligosaccharides) are covalently linked to these immunosuppressive glycoproteins and act as "functional groups" that suppress the immune response. The major uterine and fetal glycoproteins that are associated with the eu-FEDS model in the human include alpha-fetoprotein, CA125, and glycodelin-A (also known as placental protein 14).
Regulatory T cells also likely play a role. [11] As a fetus forms, it is seen similarly to an organ transplant due to it being semi-allogenic, having genetic material different to the mother. [12] Since the fetus has partial paternal genetic material, it inherits paternal flags, called HLA alleles, that trigger the maternal adaptive immune system [13] and are responded to by fighter Cytotoxic T cells and peacekeeping Regulatory T cells (Treg). [14] In order for the foreign paternal fetal material to be accepted and unharmed by the maternal immune system, the Regulatory T-cells must keep a balance with the cytotoxic T-cells, overriding autoimmune attacks.
Another participant in the balance of both T-cells is Indoleamine 2,3-dioxygenase (IDO) [13] which originates from Trophoblast cells and causes cell cycle arrest in T-cells, preventing them from differentiating into effector or fighter T-cells. [15] IDO is transformed by factors produced by Trophoblast cells [16] and suppresses T-cell activation. [13] Results from a study reveals that women with recurrent pregnancy loss have reduced levels of Treg cells. [13] This shows that insufficient Treg cells are unable to balance cytotoxic T cells and their attacks, causing the maternal immune system to treat fetal material as foreign, destroying it.
Also, a shift from cell-mediated immunity toward humoral immunity is believed to occur. [17]