Related Research Articles

Magnetic resonance imaging (MRI) is a medical imaging technique used in radiology to form pictures of the anatomy and the physiological processes inside the body. MRI scanners use strong magnetic fields, magnetic field gradients, and radio waves to generate images of the organs in the body. MRI does not involve X-rays or the use of ionizing radiation, which distinguishes it from computed tomography (CT) and positron emission tomography (PET) scans. MRI is a medical application of nuclear magnetic resonance (NMR) which can also be used for imaging in other NMR applications, such as NMR spectroscopy.

Neurosurgery or neurological surgery, known in common parlance as brain surgery, is the medical specialty concerned with the surgical treatment of disorders which affect any portion of the nervous system including the brain, spinal cord and peripheral nervous system.

A brain tumor occurs when abnormal cells form within the brain. There are two main types of tumors: malignant (cancerous) tumors and benign (non-cancerous) tumors. These can be further classified as primary tumors, which start within the brain, and secondary tumors, which most commonly have spread from tumors located outside the brain, known as brain metastasis tumors. All types of brain tumors may produce symptoms that vary depending on the size of the tumor and the part of the brain that is involved. Where symptoms exist, they may include headaches, seizures, problems with vision, vomiting and mental changes. Other symptoms may include difficulty walking, speaking, with sensations, or unconsciousness.
Image-guided surgery (IGS) is any surgical procedure where the surgeon uses tracked surgical instruments in conjunction with preoperative or intraoperative images in order to directly or indirectly guide the procedure. Image guided surgery systems use cameras, ultrasonic, electromagnetic or a combination of fields to capture and relay the patient's anatomy and the surgeon's precise movements in relation to the patient, to computer monitors in the operating room or to augmented reality headsets. This is generally performed in real-time though there may be delays of seconds or minutes depending on the modality and application.
Intraoperative neurophysiological monitoring (IONM) or intraoperative neuromonitoring is the use of electrophysiological methods such as electroencephalography (EEG), electromyography (EMG), and evoked potentials to monitor the functional integrity of certain neural structures during surgery. The purpose of IONM is to reduce the risk to the patient of iatrogenic damage to the nervous system, and/or to provide functional guidance to the surgeon and anesthesiologist.

Oligoastrocytomas are a subset of brain tumors that present with an appearance of mixed glial cell origin, astrocytoma and oligodendroglioma. However, the term "Oligoastrocytoma" is now considered obsolete by the National Comprehensive Cancer Network stating "the term should no longer be used as such morphologically ambiguous tumors can be reliably resolved into astrocytomas and oligodendrogliomas with molecular testing."
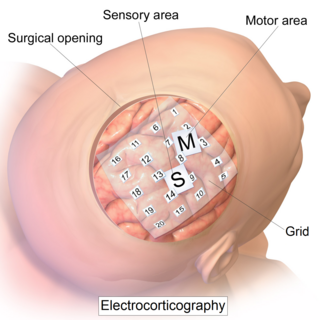
Electrocorticography (ECoG), a type of intracranial electroencephalography (iEEG), is a type of electrophysiological monitoring that uses electrodes placed directly on the exposed surface of the brain to record electrical activity from the cerebral cortex. In contrast, conventional electroencephalography (EEG) electrodes monitor this activity from outside the skull. ECoG may be performed either in the operating room during surgery or outside of surgery. Because a craniotomy is required to implant the electrode grid, ECoG is an invasive procedure.

A sphenoid wing meningioma is a benign brain tumor near the sphenoid bone.

Brain biopsy is the removal of a small piece of brain tissue for the diagnosis of abnormalities of the brain. It is used to diagnose tumors, infection, inflammation, and other brain disorders. By examining the tissue sample under a microscope, the biopsy sample provides information about the appropriate diagnosis and treatment.

Interventional magnetic resonance imaging, also interventional MRI or IMRI, is the use of magnetic resonance imaging (MRI) to do interventional radiology procedures.
NeuroArm is an engineering research surgical robot specifically designed for neurosurgery. It is the first image-guided, MR-compatible surgical robot that has the capability to perform both microsurgery and stereotaxy.
Intraoperative electron radiation therapy is the application of electron radiation directly to the residual tumor or tumor bed during cancer surgery. Electron beams are useful for intraoperative radiation treatment because, depending on the electron energy, the dose falls off rapidly behind the target site, therefore sparing underlying healthy tissue.
Computer-assisted surgery (CAS) represents a surgical concept and set of methods, that use computer technology for surgical planning, and for guiding or performing surgical interventions. CAS is also known as computer-aided surgery, computer-assisted intervention, image-guided surgery, digital surgery and surgical navigation, but these are terms that are more or less synonymous with CAS. CAS has been a leading factor in the development of robotic surgery.
An MRI robot is a medical robot capable of operating within a magnetic resonance imaging (MRI) scanner for the purpose of performing or assisting in image-guided interventions (IGI).

Magnetic resonance neurography (MRN) is the direct imaging of nerves in the body by optimizing selectivity for unique MRI water properties of nerves. It is a modification of magnetic resonance imaging. This technique yields a detailed image of a nerve from the resonance signal that arises from in the nerve itself rather than from surrounding tissues or from fat in the nerve lining. Because of the intraneural source of the image signal, the image provides a medically useful set of information about the internal state of the nerve such as the presence of irritation, nerve swelling (edema), compression, pinch or injury. Standard magnetic resonance images can show the outline of some nerves in portions of their courses but do not show the intrinsic signal from nerve water. Magnetic resonance neurography is used to evaluate major nerve compressions such as those affecting the sciatic nerve (e.g. piriformis syndrome), the brachial plexus nerves (e.g. thoracic outlet syndrome), the pudendal nerve, or virtually any named nerve in the body. A related technique for imaging neural tracts in the brain and spinal cord is called magnetic resonance tractography or diffusion tensor imaging.

A hybrid operating room is a very advanced surgical theatre that is equipped with advanced medical imaging devices such as fixed C-Arms, X-ray tomography (CT) scanners or magnetic resonance imaging (MRI) scanners. These imaging devices enable minimally-invasive surgery. Minimally-invasive surgery is intended to be less traumatic for the patient and minimize incisions on the patient and perform surgery procedure through one or several small cuts.
Endoscopic endonasal surgery is a minimally invasive technique used mainly in neurosurgery and otolaryngology. A neurosurgeon or an otolaryngologist, using an endoscope that is entered through the nose, fixes or removes brain defects or tumors in the anterior skull base. Normally an otolaryngologist performs the initial stage of surgery through the nasal cavity and sphenoid bone; a neurosurgeon performs the rest of the surgery involving drilling into any cavities containing a neural organ such as the pituitary gland. The use of endoscope was first introduced in Transsphenoidal Pituitary Surgery by R Jankowsky, J Auque, C Simon et al. in 1992 G.
The Dextroscope is a medical equipment system that creates a virtual reality (VR) environment in which surgeons can plan neurosurgical and other surgical procedures.

Ferenc Andras Jolesz was a Hungarian-American physician and scientist best known for his research on image guided therapy, the process by which information derived from diagnostic imaging is used to improve the localization and targeting of diseased tissue to monitor and control treatment during surgical and interventional procedures. He pioneered the field of Magnetic Resonance Imaging-guided interventions and introduced of a variety of new medical procedures based on novel combinations of imaging and therapy delivery.
Awake craniotomy is a neurosurgical technique and type of craniotomy that allows a surgeon to remove a brain tumor while the patient is awake to avoid brain damage. During the surgery, the neurosurgeon performs cortical mapping to identify vital areas, called the "eloquent brain", that should not be disturbed while removing the tumor.
References
- 1 2 3 4 Chicoine MR, Lim CC, et al. 2011. Implementation and preliminary clinical experience with the use of ceiling mounted mobile high field intraoperative magnetic resonance imaging between two operating rooms. Acta Neurochir Suppl. 2011:109:97-102
- 1 2 3 Winder MJ; et al. (2011). "The Evolution of Intraoperative Imaging and Neuro-Navigation in Transsphenoidal Surgery". J. Surg. Rad. 2 (1): 58–67.
- 1 2 M Bergsneider and LM Liau. 2006. Intraoperative Magnetic Resonance Imaging for Brain Tumor Resection. Ch. 13: 104-113. In, Neurosurgical Operative Atlas, Second Edition
- 1 2 Mislow JM, Golby AJ, Black PM (2009). "Origins of iMRI". Neurosurg. Clin. N. Am. 20 (2): 137–146. doi:10.1016/j.nec.2009.04.002. PMC 2902263 . PMID 19555875.
- ↑ E Yeates. Sept. 14, 2011. MRI on Rails Opening New Doors for Brain Tumor Patients, KSL-TV; http://www.ksl.com/?nid=148&sid=17247449
- ↑ W Weir. Sept. 7, 2012. New Technology Helps Doctors Remove Dangerous Clot from Girl’s brain, Hartford Courant
- ↑ N Sanai, MS Berger. 2009. Operative techniques for gliomas and the value of extent of resection. Neurotherapeutics 6(3):478-86