Angiography or arteriography is a medical imaging technique used to visualize the inside, or lumen, of blood vessels and organs of the body, with particular interest in the arteries, veins, and the heart chambers. Modern angiography is performed by injecting a radio-opaque contrast agent into the blood vessel and imaging using X-ray based techniques such as fluoroscopy.

Optical coherence tomography (OCT) is an imaging technique that uses interferometry with short-coherence-length light to obtain micrometer-level depth resolution and uses transverse scanning of the light beam to form two- and three-dimensional images from light reflected from within biological tissue or other scattering media. Short-coherence-length light can be obtained using a superluminescent diode (SLD) with a broad spectral bandwidth or a broadly tunable laser with narrow linewidth. The first demonstration of OCT imaging was published by a team from MIT and Harvard Medical School in a 1991 article in the journal Science. The article introduced the term "OCT" to credit its derivation from optical coherence-domain reflectometry, in which the axial resolution is based on temporal coherence. The first demonstrations of in vivo OCT imaging quickly followed.

An atheroma, or atheromatous plaque, is an abnormal accumulation of material in the inner layer of an arterial wall.
Intravascular ultrasound (IVUS) or intravascular echocardiography is a medical imaging methodology using a specially designed catheter with a miniaturized ultrasound probe attached to the distal end of the catheter. The proximal end of the catheter is attached to computerized ultrasound equipment. It allows the application of ultrasound technology, such as piezoelectric transducer or CMUT, to see from inside blood vessels out through the surrounding blood column, visualizing the endothelium of blood vessels.

Percutaneous coronary intervention (PCI) is a minimally invasive non-surgical procedure used to treat narrowing of the coronary arteries of the heart found in coronary artery disease. The procedure is used to place and deploy coronary stents, a permanent wire-meshed tube, to open narrowed coronary arteries. PCI is considered 'non-surgical' as it uses a small hole in a peripheral artery (leg/arm) to gain access to the arterial system, an equivalent surgical procedure would involve the opening of the chest wall to gain access to the heart area. The term 'coronary angioplasty with stent' is synonymous with PCI. The procedure visualises the blood vessels via fluoroscopic imaging and contrast dyes. PCI is performed by an interventional cardiologists in a catheterization laboratory setting.

A drug-eluting stent (DES) is a tube made of a mesh-like material used to treat narrowed arteries in medical procedures both mechanically and pharmacologically. A DES is inserted into a narrowed artery using a delivery catheter usually inserted through a larger artery in the groin or wrist. The stent assembly has the DES mechanism attached towards the front of the stent, and usually is composed of the collapsed stent over a collapsed polymeric balloon mechanism, the balloon mechanism is inflated and used to expand the meshed stent once in position. The stent expands, embedding into the occluded artery wall, keeping the artery open, thereby improving blood flow. The mesh design allows for stent expansion and also for new healthy vessel endothelial cells to grow through and around it, securing it in place.
The history of invasive and interventional cardiology is complex, with multiple groups working independently on similar technologies. Invasive and interventional cardiology is currently closely associated with cardiologists, though the development and most of its early research and procedures were performed by diagnostic and interventional radiologists.
Fractional flow reserve (FFR) is a diagnostic technique used in coronary catheterization. FFR measures pressure differences across a coronary artery stenosis to determine the likelihood that the stenosis impedes oxygen delivery to the heart muscle.

Intima–media thickness (IMT), also called intimal medial thickness, is a measurement of the thickness of tunica intima and tunica media, the innermost two layers of the wall of an artery. The measurement is usually made by external ultrasound and occasionally by internal, invasive ultrasound catheters. Measurements of the total wall thickness of blood vessels can also be done using other imaging modalities.
A coronary CT calcium scan is a computed tomography (CT) scan of the heart for the assessment of severity of coronary artery disease. Specifically, it looks for calcium deposits in atherosclerotic plaques in the coronary arteries that can narrow arteries and increase the risk of heart attack. These plaques are the cause of most heart attacks, and become calcified as they develop.

A coronary stent is a tube-shaped device placed in the coronary arteries that supply blood to the heart, to keep the arteries open in patients suffering from coronary heart disease. The vast majority of stents used in modern interventional cardiology are drug-eluting stents (DES). They are used in a medical procedure called percutaneous coronary intervention (PCI). Coronary stents are divided into two broad types: drug-eluting and bare metal stents. As of 2023, drug-eluting stents were used in more than 90% of all PCI procedures. Stents reduce angina and have been shown to improve survival and decrease adverse events after a patient has suffered a heart attack—medically termed an acute myocardial infarction.

Coronary artery aneurysm is an abnormal dilatation of part of the coronary artery. This rare disorder occurs in about 0.3–4.9% of patients who undergo coronary angiography.

Atherectomy is a minimally invasive technique for removing atherosclerosis from blood vessels within the body. It is an alternative to angioplasty for the treatment of peripheral artery disease, but the studies that exist are not adequate to determine whether it is superior to angioplasty. It has also been used to treat coronary artery disease, albeit without evidence of superiority to angioplasty.

Spontaneous coronary artery dissection (SCAD) is an uncommon but potentially lethal condition in which one of the coronary arteries that supply the heart, spontaneously develops a blood collection, or hematoma, within the artery wall due to a tear in the wall. SCAD is one of the arterial dissections that can occur.

Coronary CT angiography is the use of computed tomography (CT) angiography to assess the coronary arteries of the heart. The patient receives an intravenous injection of radiocontrast and then the heart is scanned using a high speed CT scanner, allowing physicians to assess the extent of occlusion in the coronary arteries, usually in order to diagnose coronary artery disease.
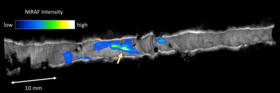
Multi-spectral optoacoustic tomography (MSOT), also known as functional photoacoustic tomography (fPAT), is an imaging technology that generates high-resolution optical images in scattering media, including biological tissues. MSOT illuminates tissue with light of transient energy, typically light pulses lasting 1-100 nanoseconds. The tissue absorbs the light pulses, and as a result undergoes thermo-elastic expansion, a phenomenon known as the optoacoustic or photoacoustic effect. This expansion gives rise to ultrasound waves (photoechoes) that are detected and formed into an image. Image formation can be done by means of hardware or computed tomography. Unlike other types of optoacoustic imaging, MSOT involves illuminating the sample with multiple wavelengths, allowing it to detect ultrasound waves emitted by different photoabsorbing molecules in the tissue, whether endogenous or exogenous. Computational techniques such as spectral unmixing deconvolute the ultrasound waves emitted by these different absorbers, allowing each emitter to be visualized separately in the target tissue. In this way, MSOT can allow visualization of hemoglobin concentration and tissue oxygenation or hypoxia. Unlike other optical imaging methods, MSOT is unaffected by photon scattering and thus can provide high-resolution optical images deep inside biological tissues.
Giovanni J. Ughi, engineer and scientist, is one of the inventors of multimodality optical coherence tomography (OCT) and Laser-induced fluorescence molecular imaging, pioneering a first-in-man study of coronary arteries during his work at Massachusetts General Hospital and Harvard Medical School. The results of his work, combining two imaging technologies, may better identify dangerous coronary plaques, responsible for coronary artery disease and myocardial infarction.

Endoscopic optical coherence tomography, also intravascular optical coherence tomography is a catheter-based imaging application of optical coherence tomography (OCT). It is capable of acquiring high-resolution images from inside a blood vessel using optical fibers and laser technology.
Intravascular imaging is a catheter based system that allows physicians such as interventional cardiologists to acquire images of diseased vessels from inside the artery. Intravascular imaging provides detailed and accurate measurements of vessel lumen morphology, vessel size, extension of diseased artery segments, vessel size and plaque characteristics. Examples of intravascular imaging modalities are intravascular ultrasound (IVUS) and intracoronary optical coherence tomography.
Blood vessel disorder generally refers to the narrowing, hardening or enlargement of arteries and veins. It is often due to the build-up of fatty deposits in the lumen of blood vessels or infection of the vessel wall. This can occur in various locations such as coronary blood vessels, peripheral arteries and veins. The narrowed arteries would block the blood supply to different organs and tissues. In severe conditions, it may develop into more critical health problems like myocardial infarction, stroke or heart failure, which are some of the major reasons of death.