Related Research Articles
Hemolysis or haemolysis, also known by several other names, is the rupturing (lysis) of red blood cells (erythrocytes) and the release of their contents (cytoplasm) into surrounding fluid. Hemolysis may occur in vivo or in vitro.

Hemoglobinopathy is the medical term for a group of inherited blood disorders and diseases that primarily affect red blood cells. They are single-gene disorders and, in most cases, they are inherited as autosomal co-dominant traits.

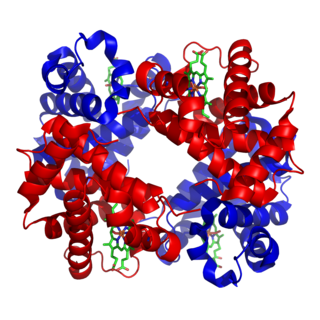
Haptoglobin is the protein that in humans is encoded by the HP gene. In blood plasma, haptoglobin binds with high affinity to free hemoglobin released from erythrocytes, and thereby inhibits its deleterious oxidative activity. Compared to Hp, hemopexin binds to free heme. The haptoglobin-hemoglobin complex will then be removed by the reticuloendothelial system.

Hereditary spherocytosis (HS) is a congenital hemolytic disorder, wherein a genetic mutation coding for a structural membrane protein phenotype leads to a spherical shaping of erythrocytic cellular morphology. As erythrocytes are sphere-shaped (spherocytosis), rather than the normal biconcave disk-shaped, their morphology interferes with these cells' abilities to be flexible during circulation throughout the entirety of the body - arteries, arterioles, capillaries, venules, veins, and organs. This difference in shape also makes the red blood cells more prone to rupture under osmotic and/or mechanical stress. Cells with these dysfunctional proteins are degraded in the spleen, which leads to a shortage of erythrocytes resulting in hemolytic anemia.

Paroxysmal nocturnal hemoglobinuria (PNH) is a rare, acquired, life-threatening disease of the blood characterized by destruction of red blood cells by the complement system, a part of the body's innate immune system. This destructive process occurs due to deficiency of the red blood cell surface protein DAF, which normally inhibits such immune reactions. Since the complement cascade attacks the red blood cells within the blood vessels of the circulatory system, the red blood cell destruction (hemolysis) is considered an intravascular hemolytic anemia. Other key features of the disease, such as the high incidence of venous blood clot formation, are incompletely understood.

Hemolytic anemia is a form of anemia due to hemolysis, the abnormal breakdown of red blood cells (RBCs), either in the blood vessels or elsewhere in the human body (extravascular). This most commonly occurs within the spleen, but also can occur in the reticuloendothelial system or mechanically. Hemolytic anemia accounts for 5% of all existing anemias. It has numerous possible consequences, ranging from general symptoms to life-threatening systemic effects. The general classification of hemolytic anemia is either intrinsic or extrinsic. Treatment depends on the type and cause of the hemolytic anemia.
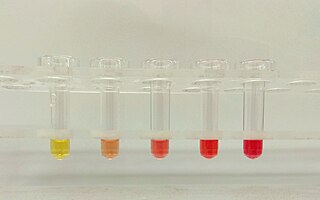
Hemoglobinuria is a condition in which the oxygen transport protein hemoglobin is found in abnormally high concentrations in the urine. The condition is caused by excessive intravascular hemolysis, in which large numbers of red blood cells (RBCs) are destroyed, thereby releasing free hemoglobin into the plasma. Excess hemoglobin is filtered by the kidneys, which excrete it into the urine, giving urine a purple color. Hemoglobinuria can lead to acute tubular necrosis which is an uncommon cause of a death of uni-traumatic patients recovering in the ICU.

Hemopexin, also known as beta-1B-glycoprotein, is a glycoprotein that in humans is encoded by the HPX gene and belongs to the hemopexin family of proteins. Hemopexin is the plasma protein with the highest binding affinity for heme.
Autoimmune hemolytic anemia (AIHA) occurs when antibodies directed against the person's own red blood cells (RBCs) cause them to burst (lyse), leading to an insufficient number of oxygen-carrying red blood cells in the circulation. The lifetime of the RBCs is reduced from the normal 100–120 days to just a few days in serious cases. The intracellular components of the RBCs are released into the circulating blood and into tissues, leading to some of the characteristic symptoms of this condition. The antibodies are usually directed against high-incidence antigens, therefore they also commonly act on allogenic RBCs. AIHA is a relatively rare condition, with an incidence of 5-10 cases per 1 million persons per year in the warm-antibody type and 0.45 to 1.9 cases per 1 million persons per year in the cold antibody type. Autoimmune hemolysis might be a precursor of later onset systemic lupus erythematosus.
Paroxysmal cold hemoglobinuria (PCH) is an autoimmune hemolytic anemia featured by complement-mediated intravascular hemolysis after cold exposure. It can present as an acute non-recurrent postinfectious event in children, or chronic relapsing episodes in adults with hematological malignancies or tertiary syphilis. Described by Julius Donath (1870–1950) and Karl Landsteiner (1868–1943) in 1904, PCH is one of the first clinical entities recognized as an autoimmune disorder.
The Schumm test(shoom) is a blood test that uses spectroscopy to determine significant levels of methemalbumin in the blood. A positive result could indicate intravascular hemolysis. The Schumm test was named for Otto Schumm, a German chemist who lived in the early 20th century.
Hemosiderinuria is the presence of hemosiderin in urine. It is often the result of chronic intravascular hemolysis, in which hemoglobin is released from red blood cells into the bloodstream in excess of the binding capacity of haptoglobin. The function of haptoglobin is to bind to circulating hemoglobin, thereby reducing renal excretion of hemoglobin and preventing injury to kidney tubules. The excess hemoglobin that is not bound to haptoglobin is filtered by the kidneys and reabsorbed in the proximal convoluted tubule, where the iron portion is removed and stored in ferritin or hemosiderin. The tubule cells of the proximal tubule become damaged, slough off with the hemosiderin and are excreted into the urine, producing a "brownish" color. It is usually seen three to four days after the onset of hemolytic conditions.

Hemoglobinemia is a medical condition in which there is an excess of hemoglobin in the blood plasma. This is an effect of intravascular hemolysis, in which hemoglobin separates from red blood cells, a form of anemia.
Hematologic diseases are disorders which primarily affect the blood & blood-forming organs. Hematologic diseases include rare genetic disorders, anemia, HIV, sickle cell disease & complications from chemotherapy or transfusions.
Normocytic anemia is a type of anemia and is a common issue that occurs for men and women typically over 85 years old. Its prevalence increases with age, reaching 44 percent in men older than 85 years. The most common type of normocytic anemia is anemia of chronic disease.
Alpha-1-microglobulin is a microglobulin, a small globular protein. It is found in all vertebrates, including humans, and is distributed in blood plasma and extravascular tissues of all organs. It is synthesized in most cells of the body, but mainly in the liver from a gene that codes for the alpha-1-microglobulin/bikunin precursor.

A urine test strip or dipstick is a basic diagnostic tool used to determine pathological changes in a patient's urine in standard urinalysis.
Sickle cell nephropathy is a type of nephropathy associated with sickle cell disease which causes kidney complications as a result of sickling of red blood cells in the small blood vessels. The hypertonic and relatively hypoxic environment of the renal medulla, coupled with the slow blood flow in the vasa recta, favors sickling of red blood cells, with resultant local infarction. Functional tubule defects in patients with sickle cell disease are likely the result of partial ischemic injury to the renal tubules.
Mechanical hemolytic anemia is a form of hemolytic anemia due to mechanically induced damage to red blood cells. Red blood cells, while flexible, may in some circumstances succumb to physical shear and compression. This may result in hemoglobinuria. The damage is induced through repetitive mechanical motions such as prolonged marching and marathon running. Mechanical damage can also be induced through the chronic condition microangiopathic hemolytic anemia or due to prosthetic heart valves.
Hemolytic jaundice, also known as prehepatic jaundice, is a type of jaundice arising from hemolysis or excessive destruction of red blood cells, when the byproduct bilirubin is not excreted by the hepatic cells quickly enough. Unless the patient is concurrently affected by hepatic dysfunctions or is experiencing hepatocellular damage, the liver does not contribute to this type of jaundice.
References
- ↑ Stanley L Schrier. William C Mentzer; Jennifer S Tirnauer (eds.). "Diagnosis of hemolytic anemia in the adult". UpToDate. Archived from the original on 2017-12-26. Retrieved 2019-05-04.
- 1 2 3 4 5 6 "Intravascular hemolysis". eClinpath. Retrieved 2019-05-08.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Muller, Andre; Jacobsen, Helene; Healy, Edel; McMickan, Sinead; Istace, Fréderique; Blaude, Marie-Noëlle; Howden, Peter; Fleig, Helmut; Schulte, Agnes (2006). "Hazard classification of chemicals inducing haemolytic anaemia: An EU regulatory perspective" (PDF). Regulatory Toxicology and Pharmacology. Elsevier BV. 45 (3): 229–241. doi:10.1016/j.yrtph.2006.04.004. hdl: 10029/5596 . ISSN 0273-2300. PMID 16793184. Archived from the original (PDF) on 2019-05-03. Retrieved 2019-05-04.
- ↑ "Bilirubin and hemolytic anemia". eClinpath. Retrieved 2019-05-08.
- 1 2 Schaer, D. J.; Buehler, P. W.; Alayash, A. I.; Belcher, J. D.; Vercellotti, G. M. (2012-12-20). "Hemolysis and free hemoglobin revisited: exploring hemoglobin and hemin scavengers as a novel class of therapeutic proteins". Blood. American Society of Hematology. 121 (8): 1276–1284. doi:10.1182/blood-2012-11-451229. ISSN 0006-4971. PMC 3578950 . PMID 23264591.
- 1 2 3 4 5 6 7 8 Rother, Russell P.; Bell, Leonard; Hillmen, Peter; Gladwin, Mark T. (2005-04-06). "The Clinical Sequelae of Intravascular Hemolysis and Extracellular Plasma Hemoglobin". JAMA. 293 (13): 1653–1662. doi: 10.1001/jama.293.13.1653 . ISSN 0098-7484. PMID 15811985.
When the capacity of protective hemoglobin-scavenging mechanisms has been saturated, levels of cell-free hemoglobin increase in the plasma, resulting in the consumption of nitric oxide and clinical sequelae.
- ↑ Schaer, Dominik J.; Vinchi, Francesca; Ingoglia, Giada; Tolosano, Emanuela; Buehler, Paul W. (2014-10-28). "Haptoglobin, hemopexin, and related defense pathwaysâ€"basic science, clinical perspectives, and drug development". Frontiers in Physiology. Frontiers Media SA. 5: 415. doi: 10.3389/fphys.2014.00415 . ISSN 1664-042X. PMC 4211382 . PMID 25389409.
- ↑ Kaushansky, Kenneth (2015). Williams hematology. New York: McGraw-Hill. ISBN 978-0-07-183300-4. OCLC 913870019.