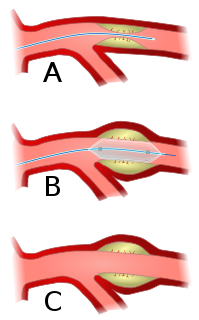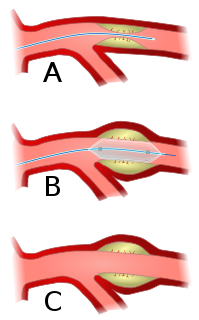
Angioplasty, is also known as balloon angioplasty and percutaneous transluminal angioplasty (PTA), is a minimally invasive endovascular procedure used to widen narrowed or obstructed arteries or veins, typically to treat arterial atherosclerosis. A deflated balloon attached to a catheter is passed over a guide-wire into the narrowed vessel and then inflated to a fixed size. The balloon forces expansion of the blood vessel and the surrounding muscular wall, allowing an improved blood flow. A stent may be inserted at the time of ballooning to ensure the vessel remains open, and the balloon is then deflated and withdrawn. Angioplasty has come to include all manner of vascular interventions that are typically performed percutaneously.

Aortic stenosis is the narrowing of the exit of the left ventricle of the heart, such that problems result. It may occur at the aortic valve as well as above and below this level. It typically gets worse over time. Symptoms often come on gradually with a decreased ability to exercise often occurring first. If heart failure, loss of consciousness, or heart related chest pain occur due to AS the outcomes are worse. Loss of consciousness typically occurs with standing or exercising. Signs of heart failure include shortness of breath especially when lying down, at night, or with exercise, and swelling of the legs. Thickening of the valve without narrowing is known as aortic sclerosis.

An echocardiography, echocardiogram, cardiac echo or simply an echo, is an ultrasound of the heart. It is a type of medical imaging of the heart, using standard ultrasound or Doppler ultrasound.

Angiography or arteriography is a medical imaging technique used to visualize the inside, or lumen, of blood vessels and organs of the body, with particular interest in the arteries, veins, and the heart chambers. This is traditionally done by injecting a radio-opaque contrast agent into the blood vessel and imaging using X-ray based techniques such as fluoroscopy.

Interventional radiology (IR) is a medical subspecialty that performs various minimally-invasive procedures using medical imaging guidance, such as x-ray fluoroscopy, computed tomography, magnetic resonance imaging, or ultrasound. IR performs both diagnostic and therapeutic procedures through very small incisions or body orifices. Diagnostic IR procedures are those intended to help make a diagnosis or guide further medical treatment, and include image-guided biopsy of a tumor or injection of an imaging contrast agent into a hollow structure, such as a blood vessel or a duct. By contrast, therapeutic IR procedures provide direct treatment—they include catheter-based medicine delivery, medical device placement, and angioplasty of narrowed structures.

A coronary catheterization is a minimally invasive procedure to access the coronary circulation and blood filled chambers of the heart using a catheter. It is performed for both diagnostic and interventional (treatment) purposes.

dextro-Transposition of the great arteries, is a potentially life-threatening birth defect in the large arteries of the heart. The primary arteries are transposed.

Interventional cardiology is a branch of cardiology that deals specifically with the catheter based treatment of structural heart diseases. Andreas Gruentzig is considered the father of interventional cardiology after the development of angioplasty by interventional radiologist Charles Dotter.
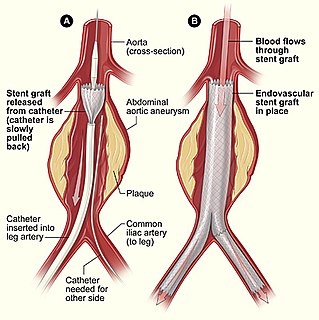
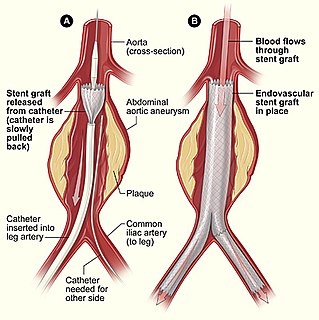
Minimally invasive procedures encompass surgical techniques that limit the size of incisions needed and so lessen wound healing time, associated pain and risk of infection. Surgery by definition is invasive and many operations requiring incisions of some size are referred to as open surgery, in which incisions made can sometimes leave large wounds that are painful and take a long time to heal. Minimally invasive procedures have been enabled by the advance of various medical technologies. An endovascular aneurysm repair as an example of minimally invasive surgery is much less invasive in that it involves much smaller incisions than the corresponding open surgery procedure of open aortic surgery. This minimally invasive surgery became the most common method of repairing abdominal aortic aneurysms in 2003 in the United States.

Cardiac catheterization is the insertion of a catheter into a chamber or vessel of the heart. This is done both for diagnostic and interventional purposes.

Percutaneous coronary intervention (PCI) is a non-surgical procedure used to treat narrowing of the coronary arteries of the heart found in coronary artery disease. The process involves combining coronary angioplasty with stenting, which is the insertion of a permanent wire-meshed tube that is either drug eluting (DES) or composed of bare metal (BMS). The stent delivery balloon from the angioplasty catheter is inflated with media to force contact between the struts of the stent and the vessel wall, thus widening the blood vessel diameter. After accessing the blood stream through the femoral or radial artery, the procedure uses coronary catheterization to visualise the blood vessels on X-ray imaging. After this, an interventional cardiologist can perform a coronary angioplasty, using a balloon catheter in which a deflated balloon is advanced into the obstructed artery and inflated to relieve the narrowing; certain devices such as stents can be deployed to keep the blood vessel open. Various other procedures can also be performed.

Arterial switch operation (ASO) or arterial switch, is an open heart surgical procedure used to correct dextro-transposition of the great arteries (d-TGA); its development was pioneered by Canadian cardiac surgeon William Mustard and it was named for Brazilian cardiac surgeon Adib Jatene, who was the first to use it successfully. It was the first method of d-TGA repair to be attempted, but the last to be put into regular use because of technological limitations at the time of its conception.
A medical procedure is a course of action intended to achieve a result in the delivery of healthcare.
Alcohol septal ablation (ASA) is a percutaneous, minimally invasive procedure performed by an interventional cardiologist to relieve symptoms and improve functional status in eligible patients with severely symptomatic hypertrophic cardiomyopathy (HCM) who meet strict clinical, anatomic and physiologic selection criteria. In carefully selected patients, when performed by an experienced interventional cardiologist, the procedure is successful in relieving symptoms in over 90% of patients.

Computed tomography angiography is a computed tomography technique used for angiography — the visualization of arteries and veins — throughout the human body. Using contrast injected into the blood vessels, images are created to look for blockages, aneurysms, dissections, and stenosis. CTA can be used to visualize the vessels of the heart, the aorta and other large blood vessels, the lungs, the kidneys, the head and neck, and the arms and legs.

Lutembacher's syndrome is a very rare form of congenital heart disease that affects one of the chambers of the heart as well as a valve. It is commonly known as both congenital atrial septal defect (ASD) and acquired mitral stenosis (MS). Congenital atrial septal defect refers to a hole being in the septum or wall that separates the two atria; this condition is usually seen in fetuses and infants. Mitral stenosis refers to mitral valve leaflets sticking to each other making the opening for blood to pass from the atrium to the ventricles very small. With the valve being so small, blood has difficulty passing from the left atrium into the left ventricle. Septal defects that may occur with Lutembacher's syndrome include: Ostium primum atrial septal defect or ostium secundum which is more prevalent.

A coronary stent is a tube-shaped device placed in the coronary arteries that supply blood to the heart, to keep the arteries open in the treatment of coronary heart disease. It is used in a procedure called percutaneous coronary intervention (PCI). Coronary stents are now used in more than 90% of PCI procedures. Stents reduce angina and have been shown to improve survivability and decrease adverse events in an acute myocardial infarction.

Atrial septostomy is a surgical procedure in which a small hole is created between the upper two chambers of the heart, the atria. This procedure is primarily used to palliate dextro-Transposition of the great arteries or d-TGA, a life-threatening cyanotic congenital heart defect seen in infants. It is performed prior to an arterial switch operation. Atrial septostomy has also seen limited use as a surgical treatment for pulmonary hypertension. The first atrial septostomy was developed by Vivien Thomas in a canine model and performed in humans by Alfred Blalock. The Rashkind balloon procedure, a common atrial septostomy technique, was developed in 1966 by American cardiologist William Rashkind at the Children's Hospital of Philadelphia.

A hybrid cardiac surgical procedure in a narrow sense is defined as a procedure that combines a conventional, more invasive surgical part with an interventional part, using some sort of catheter-based procedure guided by fluoroscopy imaging in a hybrid operating room (OR) without interruption. The hybrid technique has a reduced risk of surgical complications and has shown decreased recovery time. It can be used to treat numerous heart diseases and conditions and with the increasing complexity of each case, the hybrid surgical technique is becoming more common.
Percutaneous pulmonary valve implantation (PPVI), also known as transcatheter pulmonary valve replacement (TPVR), is the replacement of the pulmonary valve via catheterization through a vein. It is a significantly less invasive procedure in comparison to open heart surgery and is commonly used to treat conditions such as pulmonary atresia.