Related Research Articles
Periodontal disease, also known as gum disease, is a set of inflammatory conditions affecting the tissues surrounding the teeth. In its early stage, called gingivitis, the gums become swollen and red and may bleed. It is considered the main cause of tooth loss for adults worldwide. In its more serious form, called periodontitis, the gums can pull away from the tooth, bone can be lost, and the teeth may loosen or fall out. Bad breath may also occur.

Endodontics is the dental specialty concerned with the study and treatment of the dental pulp.

Toothache, also known as dental pain, is pain in the teeth or their supporting structures, caused by dental diseases or pain referred to the teeth by non-dental diseases. When severe it may impact sleep, eating, and other daily activities.

The pulp is the connective tissue, nerves, blood vessels, and odontoblasts that comprise the innermost layer of a tooth. The pulp's activity and signalling processes regulate its behaviour.
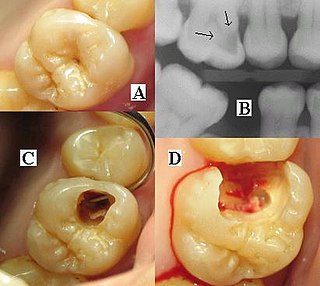
A pulp polyp, also known as chronic hyperplastic pulpitis, is a "productive" inflammation of dental pulp in which the development of granulation tissue is seen in response to persistent, low-grade mechanical irritation and bacterial invasion of the pulp.

A dental abscess is a localized collection of pus associated with a tooth. The most common type of dental abscess is a periapical abscess, and the second most common is a periodontal abscess. In a periapical abscess, usually the origin is a bacterial infection that has accumulated in the soft, often dead, pulp of the tooth. This can be caused by tooth decay, broken teeth or extensive periodontal disease. A failed root canal treatment may also create a similar abscess.
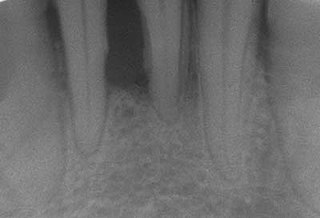
Dental radiographs, commonly known as X-rays, are radiographs used to diagnose hidden dental structures, malignant or benign masses, bone loss, and cavities.

Root canal treatment is a treatment sequence for the infected pulp of a tooth which is intended to result in the elimination of infection and the protection of the decontaminated tooth from future microbial invasion. Root canals, and their associated pulp chamber, are the physical hollows within a tooth that are naturally inhabited by nerve tissue, blood vessels and other cellular entities. Together, these items constitute the dental pulp.
Apical periodontitis is typically the body's defense response to the threat of microbial invasion from the root canal. Primary among the members of the host defense mechanism is the polymorphonuclear leukocyte, otherwise known as the neutrophil. The task of the neutrophil is to locate and destroy microbes that intrude into the body – anywhere in the body – and they represent the hallmark of acute inflammation.

Barodontalgia, commonly known as tooth squeeze, is a pain in a tooth caused by a change in ambient pressure. The pain usually ceases at ground level. Dental barotrauma is a condition in which such changes in barometric pressure changes cause damage to the dentition.

Resorption of the root of the tooth, or root resorption, is the progressive loss of dentin and cementum by the action of odontoclasts. Root resorption is a normal physiological process that occurs in the exfoliation of the primary dentition. However, pathological root resorption occurs in the permanent or secondary dentition and sometimes in the primary dentition.

A periodontal abscess, is a localized collection of pus within the tissues of the periodontium. It is a type of dental abscess. A periodontal abscess occurs alongside a tooth, and is different from the more common periapical abscess, which represents the spread of infection from a dead tooth. To reflect this, sometimes the term "lateral (periodontal) abscess" is used. In contrast to a periapical abscess, periodontal abscesses are usually associated with a vital (living) tooth. Abscesses of the periodontium are acute bacterial infections classified primarily by location.
Pulp necrosis is a clinical diagnostic category indicating the death of the pulp and nerves of the pulp chamber and root canal of a tooth which may be due to bacterial sequelae, trauma and chemical or mechanical irritation. It is often the end result of many cases of dental trauma, caries and irreversible pulpitis.
A phoenix abscess is an acute exacerbation of a chronic periapical lesion. It is a dental abscess that can occur immediately following root canal treatment. Another cause is due to untreated necrotic pulp. It is also the result of inadequate debridement during the endodontic procedure. Risk of occurrence of a phoenix abscess is minimised by correct identification and instrumentation of the entire root canal, ensuring no missed anatomy.

Periapical periodontitis or apical periodontitis (AP) is an acute or chronic inflammatory lesion around the apex of a tooth root, most commonly caused by bacterial invasion of the pulp of the tooth. It is a likely outcome of untreated dental caries, and in such cases it can be considered a sequela in the natural history of tooth decay, irreversible pulpitis and pulpal necrosis. Other causes can include occlusal trauma due to 'high spots' after restoration work, extrusion from the tooth of root filling material, or bacterial invasion and infection from the gums. Periapical periodontitis may develop into a periapical abscess, where a collection of pus forms at the end of the root, the consequence of spread of infection from the tooth pulp, or into a periapical cyst, where an epithelial lined, fluid-filled structure forms.
Dialister pneumosintes is a nonfermentative, anaerobic, gram-negative rod that grows with small, circular, transparent, shiny, smooth colonies on blood agar. D. pneumosintes has been recovered from deep periodontal pockets, but little is known about the relationship between the organism and destructive periodontal disease.

Regenerative endodontic procedures is defined as biologically based procedures designed to replace damaged structures such as dentin, root structures, and cells of the pulp-dentin complex. This new treatment modality aims to promote normal function of the pulp. It has become an alternative to heal apical periodontitis. Regenerative endodontics is the extension of root canal therapy. Conventional root canal therapy cleans and fills the pulp chamber with biologically inert material after destruction of the pulp due to dental caries, congenital deformity or trauma. Regenerative endodontics instead seeks to replace live tissue in the pulp chamber. The ultimate goal of regenerative endodontic procedures is to regenerate the tissues and the normal function of the dentin-pulp complex.
José Freitas Siqueira Jr. was born in Miracema, Rio de Janeiro, Brazil, in October 1967. He received his DDS from Gama Filho University, Rio de Janeiro in 1989, and his endodontic certificate from Federal University of Rio de Janeiro in 1991. In 1996, he received his master's degree in microbiology and immunology from Federal University of Rio de Janeiro. He concluded his PhD in microbiology and immunology in 1998 at Federal University of Rio de Janeiro. Since 2002, Siqueira is the chairman of endodontics, director of the postgraduate program in endodontics and head of the molecular microbiology laboratory at Estácio de Sá University, in Rio de Janeiro, Brazil.
In the dental specialty of endodontics, periradicular surgery is surgery to the external root surface. Examples of periradicular surgery include apicoectomy, root resection, repair of root perforation or resorption defects, removal of broken fragments of the tooth or a filling material, and exploratory surgery to look for root fractures.
Periapical granuloma, also sometimes referred to as a radicular granuloma or apical granuloma, is an inflammation at the tip of a dead (nonvital) tooth. It is a lesion or mass that typically starts out as an epithelial lined cyst, and undergoes an inward curvature that results in inflammation of granulation tissue at the root tips of a dead tooth. This is usually due to dental caries or a bacterial infection of the dental pulp. Periapical granuloma is an infrequent disorder that has an occurrence rate between 9.3 to 87.1 percent. Periapical granuloma is not a true granuloma due to the fact that it does not contain granulomatous inflammation; however, periapical granuloma is a common term used.
References
- ↑ "Hemos encontrado una asociación, estadísticamente significativa, entre el hábito de fumar y la presencia de periodontitis apical". Gaceta Dental (in Spanish). 2014-11-28. Retrieved 2020-08-31.
- ↑ "Speakers - ESE". www.e-s-e.eu. Retrieved 2020-08-31.
- ↑ "ACADEMIA DE CIENCIAS ODONTOLÓGICAS DE ESPAÑA". www.acodes.es. Retrieved 2020-09-17.
- ↑ "Speakers - ESE". www.e-s-e.eu. Retrieved 2020-08-31.
- ↑ "Siola. Sociedad de Implantología Oral Latinoamericana - JUAN JOSE SEGURA EGEA". www.siola.org. Retrieved 2020-08-29.
- ↑ "Juan J. Segura-Egea - Google Scholar". scholar.google.com. Retrieved 2020-08-29.
- ↑ "Juan J. Segura-Egea". Dialnet (in Spanish). Retrieved 2020-08-29.
- ↑ "Juan J. Segura-Egea". Dialnet (in Spanish). Retrieved 2020-09-17.
- ↑ "La Endodoncia ha estado siempre presente en mi vida". Gaceta Dental (in Spanish). 2018-01-08. Retrieved 2020-08-29.
- ↑ "International Endodontic Journal". Wiley Online Library. Retrieved 2020-09-17.
- ↑ "La odontología española sigue demostrando su excelencia científica en la última edición del Ranking de Stanford".
- ↑ Segura‐Egea, J. J.; Gould, K.; Şen, B. Hakan; Jonasson, P.; Cotti, E.; Mazzoni, A.; Sunay, H.; Tjäderhane, L.; Dummer, P. M. H. (2018). "European Society of Endodontology position statement: the use of antibiotics in endodontics". International Endodontic Journal. 51 (1): 20–25. doi: 10.1111/iej.12781 . ISSN 1365-2591. PMID 28436043.