Arthroscopy is a minimally invasive surgical procedure on a joint in which an examination and sometimes treatment of damage is performed using an arthroscope, an endoscope that is inserted into the joint through a small incision. Arthroscopic procedures can be performed during ACL reconstruction.

The anterior cruciate ligament (ACL) is one of a pair of cruciate ligaments in the human knee. The two ligaments are also called "cruciform" ligaments, as they are arranged in a crossed formation. In the quadruped stifle joint, based on its anatomical position, it is also referred to as the cranial cruciate ligament. The term cruciate translates to cross. This name is fitting because the ACL crosses the posterior cruciate ligament to form an “X”. It is composed of strong, fibrous material and assists in controlling excessive motion. This is done by limiting mobility of the joint. The anterior cruciate ligament is one of the four main ligaments of the knee, providing 85% of the restraining force to anterior tibial displacement at 30 and 90° of knee flexion. The ACL is the most injured ligament of the four located in the knee.

Anterior cruciate ligament reconstruction is a surgical tissue graft replacement of the anterior cruciate ligament, located in the knee, to restore its function after an injury. The torn ligament can either be removed from the knee, or preserved before reconstruction an arthroscopic procedure. ACL repair is also a surgical option. This involves repairing the ACL by re-attaching it, instead of performing a reconstruction. Theoretical advantages of repair include faster recovery and a lack of donor site morbidity, but randomised controlled trials and long-term data regarding re-rupture rates using contemporary surgical techniques are lacking.
Autotransplantation is the transplantation of organs, tissues, or even particular proteins from one part of the body to another in the same person.
A meniscus transplant or meniscal transplant is a transplant of the meniscus of the knee, which separates the thigh bone (femur) from the lower leg bone (tibia). The worn or damaged meniscus is removed and is replaced with a new one from a donor. The meniscus to be transplanted is taken from a cadaver, and, as such, is known as an allograft. Meniscal transplantation is technically difficult, as it must be sized accurately for each person, positioned properly and secured to the tibial plateau. As of 2012, only a few surgeons have significant volume of experience in meniscus transplantation worldwide.
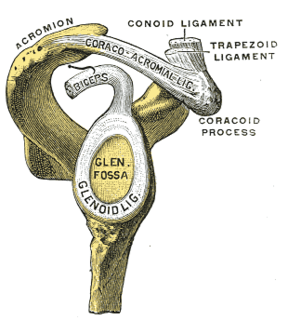
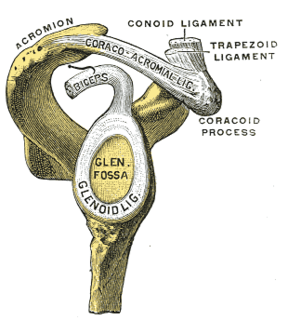
A SLAP tear or SLAP lesion is an injury to the glenoid labrum. SLAP is an acronym for "superior labral tear from anterior to posterior".
A bursectomy is the removal of a bursa, which is a small sac filled with synovial fluid that cushions adjacent bone structures and reduces friction in joint movement. This procedure is usually carried out to relieve chronic inflammation (bursitis) or infection, when conservative management has failed to improve patient outcomes.

Cranioplasty is a surgical operation on the repairing of cranial defects caused by previous injuries or operations, such as decompressive craniectomy. It is performed by filling the defective area with a range of materials, usually a bone piece from the patient or a synthetic material. Cranioplasty is carried out by incision and reflection of the scalp after applying anaesthetics and antibiotics to the patient. The temporalis muscle is reflected, and all surrounding soft tissues are removed, thus completely exposing the cranial defect. The cranioplasty flap is placed and secured on the cranial defect. The wound is then sealed.

The acetabular labrum is a ring of cartilage that surrounds the acetabulum of the hip. The anterior portion is most vulnerable when the labrum tears.

A dislocated shoulder is a condition in which the head of the humerus is detached from the shoulder joint. Symptoms include shoulder pain and instability. Complications may include a Bankart lesion, Hill-Sachs lesion, rotator cuff tear, or injury to the axillary nerve.
Shoulder surgery is a means of treating injured shoulders. Many surgeries have been developed to repair the muscles, connective tissue, or damaged joints that can arise from traumatic or overuse injuries to the shoulder.
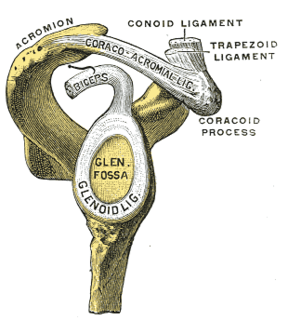
A Bankart lesion is an injury of the anterior (inferior) glenoid labrum of the shoulder. When this happens, a pocket at the front of the glenoid forms that allows the humeral head to dislocate into it. It is an indication for surgery and often accompanied by a Hill-Sachs lesion, damage to the posterior humeral head.
The aim of an articular cartilage repair treatment is to restore the surface of an articular joint's hyaline cartilage. Over the last decades, surgeons and researchers have made progress in elaborating surgical cartilage repair interventions. Though these solutions do not perfectly restore articular cartilage, some of the latest technologies start to bring very promising results in repairing cartilage from traumatic injuries or chondropathies. These treatments are especially targeted by patients who suffer from articular cartilage damage. They provide pain relief while at the same time slowing down the progression of damage or considerably delaying joint replacement surgery. Articular cartilage repair treatments help patients to return to their original lifestyle; regaining mobility, going back to work and even practicing sports again.
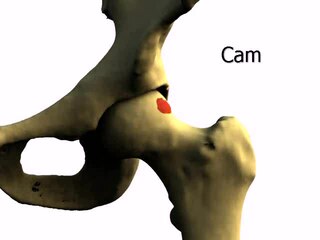
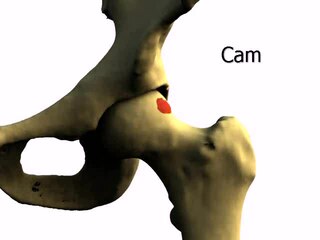
Femoroacetabular impingement (FAI) is a condition involving one or more anatomical abnormalities of the hip joint, which is a ball and socket joint. It is a common cause of hip pain and discomfort in young and middle-aged adults. It occurs when the ball shaped femoral head contacts the acetabulum abnormally or does not permit a normal range of motion in the acetabular socket. Damage can occur to the articular cartilage, or labral cartilage, or both. The condition may be symptomatic or asymptomatic. It may cause osteoarthritis of the hip. Treatment options range from conservative management to surgery.

Hip arthroscopy refers to the viewing of the interior of the acetabulofemoral (hip) joint through an arthroscope and the treatment of hip pathology through a minimally invasive approach. This technique is sometimes used to help in the treatment of various joint disorders and has gained popularity because of the small incisions used and shorter recovery times when compared with conventional surgical techniques. Hip arthroscopy was not feasible until recently, new technology in both the tools used and the ability to distract the hip joint has led to a recent surge in the ability to do hip arthroscopy and the popularity of it.
Posterolateral corner injuries of the knee are injuries to a complex area formed by the interaction of multiple structures. Injuries to the posterolateral corner can be debilitating to the person and require recognition and treatment to avoid long term consequences. Injuries to the PLC often occur in combination with other ligamentous injuries to the knee; most commonly the anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL). As with any injury, an understanding of the anatomy and functional interactions of the posterolateral corner is important to diagnosing and treating the injury.
Cartilage repair techniques are the current focus of large amounts of research. Many different strategies have been proposed as solutions for cartilage defects. Surgical techniques currently being studied include:
Nerve allotransplantation is the transplantation of a nerve to a receiver from a donor of the same species. For example, nerve tissue is transplanted from one person to another. Allotransplantation is a commonly used type of transplantation of which nerve repair is one specific aspect.

Wrist arthroscopy can be used to look inside the joint of the wrist. It is a minimally invasive technique which can be utilized for diagnostic purposes as well as for therapeutic interventions. Wrist arthroscopy has been used for diagnostic purposes since it was first introduced in 1979. However, it only became accepted as diagnostic tool around the mid-1980s. At that time, arthroscopy of the wrist was an innovative technique to determine whether a problem could be found in the wrist. A few years later, wrist arthroscopy could also be used as a therapeutic tool.

Gingival grafting, also called gum grafting or periodontal plastic surgery, is a generic term for the performance of any of a number of periodontal surgical procedures in which the gum tissue is grafted. The aim may be to cover exposed root surfaces or merely to augment the band of keratinized tissue.