Urology, also known as genitourinary surgery, is the branch of medicine that focuses on surgical and medical diseases of the urinary system and the reproductive organs. Organs under the domain of urology include the kidneys, adrenal glands, ureters, urinary bladder, urethra, and the male reproductive organs.
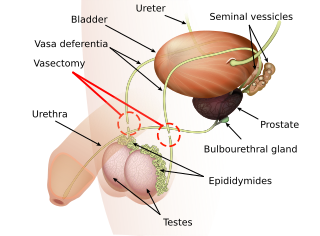
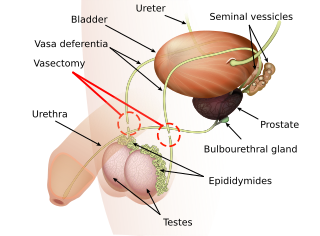
Vasectomy is an elective surgical procedure that results in male sterilization, often as a means of permanent contraception. During the procedure, the male vasa deferentia are cut and tied or sealed so as to prevent sperm from entering into the urethra and thereby prevent fertilization of a female through sexual intercourse. Vasectomies are usually performed in a physician's office, medical clinic, or, when performed on a non-human animal, in a veterinary clinic. Hospitalization is not normally required as the procedure is not complicated, the incisions are small, and the necessary equipment routine.
Andrology is a name for the medical specialty that deals with male health, particularly relating to the problems of the male reproductive system and urological problems that are unique to men. It is the parallel to gynecology, which deals with medical issues which are specific to female health, especially reproductive and urologic health.
Hypogonadism means diminished functional activity of the gonads—the testicles or the ovaries—that may result in diminished production of sex hormones. Low androgen levels are referred to as hypoandrogenism and low estrogen as hypoestrogenism. These are responsible for the observed signs and symptoms in both males and females.

Testicular atrophy is a medical condition in which one or both testicles diminish in size and may be accompanied by reduced testicular function. Testicular atrophy is not related to the temporary shrinkage of the surrounding scrotum, which might occur in response to cold temperature.

A varicocele is, in a man, an abnormal enlargement of the pampiniform venous plexus in the scrotum; in a woman, it is an abnormal painful swelling to the embryologically identical pampiniform venous plexus; it is more commonly called pelvic compression syndrome. In the male varicocele, this plexus of veins drains blood from the testicles back to the heart. The vessels originate in the abdomen and course down through the inguinal canal as part of the spermatic cord on their way to the testis. Varicoceles occur in around 15% to 20% of all men. The incidence of varicocele increase with age.
Vasovasostomy is a surgery by which vasectomies are partially reversed. Another surgery for vasectomy reversal is vasoepididymostomy.
Male infertility refers to a sexually mature male's inability to impregnate a fertile female. In humans, it accounts for 40–50% of infertility. It affects approximately 7% of all men. Male infertility is commonly due to deficiencies in the semen, and semen quality is used as a surrogate measure of male fecundity. More recently, advance sperm analyses that examine intracellular sperm components are being developed.

Reproductive medicine is a branch of medicine concerning the male and female reproductive systems. It encompasses a variety of reproductive conditions, their prevention and assessment, as well as their subsequent treatment and prognosis.
Sudhakar Krishnamurti, is a medical doctor, clinical andrologist, microsurgeon, and sexual medicine expert. He is director of the Andromeda Andrology Center, Hyderabad, India.
Post-vasectomy pain syndrome (PVPS) is a chronic and sometimes debilitating genital pain condition that may develop immediately or several years after vasectomy. Because this condition is a syndrome, there is no single treatment method, therefore efforts focus on mitigating/relieving the individual patient's specific pain. When pain in the epididymides is the primary symptom, post-vasectomy pain syndrome is often described as congestive epididymitis.
Vasectomy reversal is a term used for surgical procedures that reconnect the male reproductive tract after interruption by a vasectomy. Two procedures are possible at the time of vasectomy reversal: vasovasostomy and vasoepididymostomy. Although vasectomy is considered a permanent form of contraception, advances in microsurgery have improved the success of vasectomy reversal procedures. The procedures remain technically demanding and may not restore the pre-vasectomy condition.
Reproductive surgery is surgery in the field of reproductive medicine. It can be used for contraception, e.g. in vasectomy, wherein the vasa deferentia of a male are severed, but is also used plentifully in assisted reproductive technology. Reproductive surgery is generally divided into three categories: surgery for infertility, in vitro fertilization, and fertility preservation.

Dr. Paul J Turek is an American physician and surgeon, men's reproductive health specialist, and businessman. Turek is a recent recipient of a National Institutes of Health (NIH) grant for research designed to help infertile men become fathers using stem cells.

Sherman J. Silber is physician specializing in the field of infertility. He invented many of the infertility treatments in use today in the domain of IVF, sperm retrieval, ICSI, vasectomy reversal, tubal ligation reversal, egg and embryo freezing, ovary transplantation, and the reproductive biological clock. He performed the world's first ovary and testicle transplants, created and popularized the microsurgical vasectomy reversal, and popularized ovarian tissue freezing to preserve female fertility. He was the first to research the genetic causes of infertility in men, and developed the TESE-ICSI technique for extracting sperm from men with low or nonexistent sperm counts and direct injection of the sperm into the egg. Additionally, Silber has studied fertility in animals and performed microscopic surgery on chimpanzees, South American bush dogs, Przewalski's horse, gorillas, wolves, and other endangered species.

Ashok Agarwal is the Director of the Andrology Center, and also the Director of Research at the American Center for Reproductive Medicine at Cleveland Clinic, Cleveland, USA. He is Professor at the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University, USA. Ashok is a Senior Staff in the Cleveland Clinic's Glickman Urological and Kidney Institute. He has published extensive translational research in human infertility and assisted reproduction.

Raymond A. Costabile is Professor, and Chair Urology with the Department of Urology at the School of Medicine of the University of Virginia. Costabile is a retired Colonel in the US Army and the former Chief of Urology Service at Madigan Army Medical Center. Costabile is an author; his articles on men's reproductive health and infertility have been published in the Journal of Urology and Proceedings in the National Academy of Sciences, among other peer-reviewed scholarly journals. He has also been featured in television interviews in the national media.
Marc Goldstein is an American urologist who is the Matthew P. Hardy Distinguished Professor of Reproductive Medicine, and Urology at Weill Cornell Medical College; Surgeon-in-Chief, Male Reproductive Medicine and Surgery; and Director of the Center of Male Reproductive Medicine and Microsurgery at New York Presbyterian Hospital. He is Adjunct Senior Scientist with the Population Council's Center for Biomedical Research, located on the campus of Rockefeller University.
Ranjith Ramasamy is a consultant urologist at Jumeirah American Clinic in Dubai, UAE, and the former Director of the Reproductive Urology Fellowship program at the University of Miami's Miller School of Medicine.
Sheldon Marks is an American urologist and writer who is the founder of the International Center for Vasectomy Reversal (ICVR). He is a clinical professor at the University of Arizona College of Medicine and Assistant Professor of Urology at New England Medical Center, Tufts University.