Prescription drug list prices in the United States continually are among the highest in the world. The high cost of prescription drugs became a major topic of discussion in the 21st century, leading up to the American health care reform debate of 2009, and received renewed attention in 2015. One major reason for high prescription drug prices in the United States relative to other countries is the inability of government-granted monopolies in the American health care sector to use their bargaining power to negotiate lower prices, and the American payer ends up subsidizing the world's R&D spending on drugs.
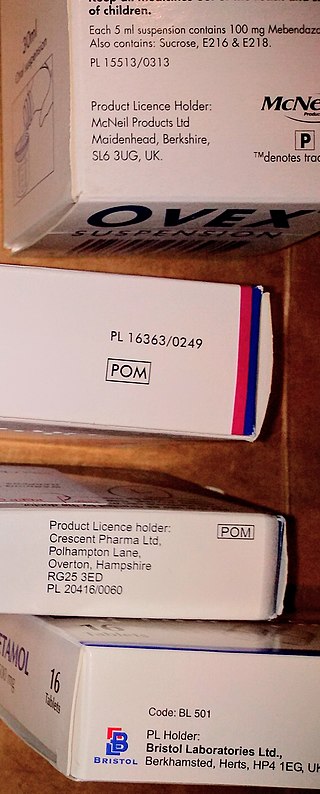
A prescription drug is a pharmaceutical drug that is permitted to be dispensed only to those with a medical prescription. In contrast, over-the-counter drugs can be obtained without a prescription. The reason for this difference in substance control is the potential scope of misuse, from drug abuse to practicing medicine without a license and without sufficient education. Different jurisdictions have different definitions of what constitutes a prescription drug.

CVS Pharmacy Inc. is an American retail corporation. A subsidiary of CVS Health, it is headquartered in Woonsocket, Rhode Island. Originally named the Consumer Value Stores, it was founded in Lowell, Massachusetts, in 1963.
Medco Health Solutions, Inc. was an American Pharmacy Benefits Management (PBM) company. Medco provided pharmacy services to private and public employers, health plans, labor unions, government agencies, and individuals served by Medicare Part D Prescription Drug Plans.

Medicare Part D, also called the Medicare prescription drug benefit, is an optional United States federal-government program to help Medicare beneficiaries pay for self-administered prescription drugs. Part D was enacted as part of the Medicare Modernization Act of 2003 and went into effect on January 1, 2006. Under the program, drug benefits are provided by private insurance plans that receive premiums from both enrollees and the government. Part D plans typically pay most of the cost for prescriptions filled by their enrollees. However, plans are later reimbursed for much of this cost through rebates paid by manufacturers and pharmacies.
Express Scripts Holding Company is a pharmacy benefit management (PBM) organization. In 2017 it was the 22nd-largest company in the United States by total revenue as well as the largest pharmacy benefit management (PBM) organization in the United States. Express Scripts had 2016 revenues of $100.752 billion. Since December 20, 2018, the company has been a direct subsidiary of Bloomfield, Connecticut-based Cigna.
In the United States, a pharmacy benefit manager (PBM) is a third-party administrator of prescription drug programs for commercial health plans, self-insured employer plans, Medicare Part D plans, the Federal Employees Health Benefits Program, and state government employee plans. PBMs operate inside of integrated healthcare systems, as part of retail pharmacies, and as part of insurance companies.
The Medicare Part D coverage gap was a period of consumer payments for prescription medication costs that lay between the initial coverage limit and the catastrophic coverage threshold when the consumer was a member of a Medicare Part D prescription-drug program administered by the United States federal government. The gap was reached after a shared insurer payment - consumer payment for all covered prescription drugs reached a government-set amount, and was left only after the consumer had paid full, unshared costs of an additional amount for the same prescriptions. Upon entering the gap, the prescription payments to date were re-set to $0 and continued until the maximum amount of the gap was reached or the then current annual period lapses. In calculating whether the maximum amount of gap had been reached, the "True-out-of-pocket" costs (TrOOP) were added together.
CVS Health Corporation is an American for-profit healthcare company that owns CVS Pharmacy, a retail pharmacy chain; CVS Caremark, a pharmacy benefits manager; and Aetna, a health insurance provider, among many other brands. The company is the world's second largest healthcare company, behind UnitedHealth Group. In 2023, the company was ranked 64th in the Forbes Global 2000.

First Databank (FDB) is a major provider of drug and medical device databases that help inform healthcare professionals to make decisions. FDB partners with information system developers to deliver useful medication- and medical device-related information to clinicians, business associates, and patients. FDB is part of Hearst and the Hearst Health network.
Medication costs, also known as drug costs are a common health care cost for many people and health care systems. Prescription costs are the costs to the end consumer. Medication costs are influenced by multiple factors such as patents, stakeholder influence, and marketing expenses. A number of countries including Canada, parts of Europe, and Brazil use external reference pricing as a means to compare drug prices and to determine a base price for a particular medication. Other countries use pharmacoeconomics, which looks at the cost/benefit of a product in terms of quality of life, alternative treatments, and cost reduction or avoidance in other parts of the health care system. Structures like the UK's National Institute for Health and Clinical Excellence and to a lesser extent Canada's Common Drug Review evaluate products in this way.
A formulary is a list of pharmaceutical drugs, often decided upon by a group of people, for various reasons such as insurance coverage or use at a medical facility. Traditionally, a formulary contained a collection of formulas for the compounding and testing of medication. Today, the main function of a prescription formulary is to specify particular medications that are approved to be prescribed at a particular hospital, in a particular health system, or under a particular health insurance policy. The development of prescription formularies is based on evaluations of efficacy, safety, and cost-effectiveness of drugs.
Electronic prescription is the computer-based electronic generation, transmission, and filling of a medical prescription, taking the place of paper and faxed prescriptions. E-prescribing allows a physician, physician assistant, pharmacist, or nurse practitioner to use digital prescription software to electronically transmit a new prescription or renewal authorization to a community or mail-order pharmacy. It outlines the ability to send error-free, accurate, and understandable prescriptions electronically from the healthcare provider to the pharmacy. E-prescribing is meant to reduce the risks associated with traditional prescription script writing. It is also one of the major reasons for the push for electronic medical records. By sharing medical prescription information, e-prescribing seeks to connect the patient's team of healthcare providers to facilitate knowledgeable decision making.
The co-pay card appeared in 2005 as a means by which pharmaceutical marketers could, by offering an instantaneous rebate to patients, combat their challenges to prescription pharmaceuticals, including generic competition, lack of patient compliance and persistency, and an access to the physician population. As of January 2017, in the United States, coupon cards for more than 600 prescription medications are available.

A drug coupon is a coupon intended to help consumers save money on pharmaceutical drugs. They are offered by drug companies or distributed to consumers via doctors and pharmacists, and most can be obtained online. There are drug coupons for drugs from many categories such as cholesterol, acne, migraine, allergies, etc.
Catamaran Corporation is the former name of a company that now operates within UnitedHealth Group's OptumRX division. It sells pharmacy benefit management and medical record keeping services to businesses in the United States and to a broad client portfolio, including health plans and employers. Working independently of the government and insurance companies allowed it to operate as a third party verifier; the RxCLAIM online claim processing system allowed for prescription drug claims to be processed online if the customer lived in and filled their prescription in the United States. SXC had three separate but interrelated business segments which dealt with prescription drug programs. For 2013, 23% of company revenue came from Cigna Corporation.
Specialty drugs or specialty pharmaceuticals are a recent designation of pharmaceuticals classified as high-cost, high complexity and/or high touch. Specialty drugs are often biologics—"drugs derived from living cells" that are injectable or infused. They are used to treat complex or rare chronic conditions such as cancer, rheumatoid arthritis, hemophilia, H.I.V. psoriasis, inflammatory bowel disease and hepatitis C. In 1990 there were 10 specialty drugs on the market, around five years later nearly 30, by 2008 200, and by 2015 300.
Specialty pharmacy refers to distribution channels designed to handle specialty drugs — pharmaceutical therapies that are either high cost, high complexity and/or high touch. High touch refers to higher degree of complexity in terms of distribution, administration, or patient management which drives up the cost of the drugs. In the early years specialty pharmacy providers attached "high-touch services to their overall price tags" arguing that patients who receive specialty pharmaceuticals "need high levels of ancillary and follow-up care to ensure that the drug spend is not wasted on them." An example of a specialty drug that would only be available through specialty pharmacy is interferon beta-1a (Avonex), a treatment for MS that requires a refrigerated chain of distribution and costs $17,000 a year. Some specialty pharmacies deal in pharmaceuticals that treat complex or rare chronic conditions such as cancer, rheumatoid arthritis, hemophilia, H.I.V. psoriasis, inflammatory bowel disease (IBD) or Hepatitis C. "Specialty pharmacies are seen as a reliable distribution channel for expensive drugs, offering patients convenience and lower costs while maximizing insurance reimbursements from those companies that cover the drug. Patients typically pay the same co-payments whether or not their insurers cover the drug." As the market demanded specialization in drug distribution and clinical management of complex therapies, specialized pharma (SP) evolved.„ Specialty pharmacies may handle therapies that are biologics, and are injectable or infused. By 2008 the pharmacy benefit management dominated the specialty pharmacies market having acquired smaller specialty pharmacies. PBMs administer specialty pharmacies in their network and can "negotiate better prices and frequently offer a complete menu of specialty pharmaceuticals and related services to serve as an attractive 'one-stop shop' for health plans and employers."
GoodRx Holdings, Inc., is an American healthcare company that operates a telemedicine platform and free-to-use website and mobile app that track prescription drug prices in the United States and provide drug coupons for discounts on medications. GoodRx checks drug prices at more than seventy-five thousand pharmacies in the United States. The platform allows individuals to consult with a doctor online and obtain a prescription for certain types of medications at a cost of US$20, regardless of insurance status. Medical testing services, which vary in price, are also offered through the platform.

The Elijah Cummings Lower Drug Costs Now Act is proposed legislation in the 117th United States Congress. The bill is designed to lower prescription drug costs in the United States. Notably, the law gives the federal government the power to negotiate prescription drug prices. The legislation takes the name of late Maryland Representative Elijah Cummings.