Related Research Articles

The blood vessels are the components of the circulatory system that transport blood throughout the human body. These vessels transport blood cells, nutrients, and oxygen to the tissues of the body. They also take waste and carbon dioxide away from the tissues. Blood vessels are needed to sustain life, because all of the body's tissues rely on their functionality.

The sympathetic nervous system (SNS) is one of two divisions of the autonomic nervous system, along with the parasympathetic nervous system. The enteric nervous system is sometimes considered part of the autonomic nervous system, and sometimes considered an independent system.

The adrenergic receptors or adrenoceptors are a class of G protein-coupled receptors that are targets of many catecholamines like norepinephrine (noradrenaline) and epinephrine (adrenaline) produced by the body, but also many medications like beta blockers, beta-2 (β2) agonists and alpha-2 (α2) agonists, which are used to treat high blood pressure and asthma, for example.

Smooth muscle is an involuntary non-striated muscle, so-called because it has no sarcomeres and therefore no striations. It is divided into two subgroups, single-unit and multiunit smooth muscle. Within single-unit muscle, the whole bundle or sheet of smooth muscle cells contracts as a syncytium.

Vasoconstriction is the narrowing of the blood vessels resulting from contraction of the muscular wall of the vessels, in particular the large arteries and small arterioles. The process is the opposite of vasodilation, the widening of blood vessels. The process is particularly important in controlling hemorrhage and reducing acute blood loss. When blood vessels constrict, the flow of blood is restricted or decreased, thus retaining body heat or increasing vascular resistance. This makes the skin turn paler because less blood reaches the surface, reducing the radiation of heat. On a larger level, vasoconstriction is one mechanism by which the body regulates and maintains mean arterial pressure.

The microcirculation is the circulation of the blood in the smallest blood vessels, the microvessels of the microvasculature present within organ tissues. The microvessels include terminal arterioles, metarterioles, capillaries, and venules. Arterioles carry oxygenated blood to the capillaries, and blood flows out of the capillaries through venules into veins.
The diving reflex, also known as the diving response and mammalian diving reflex, is a set of physiological responses to immersion that overrides the basic homeostatic reflexes, and is found in all air-breathing vertebrates studied to date. It optimizes respiration by preferentially distributing oxygen stores to the heart and brain, enabling submersion for an extended time.

Vasodilation is the widening of blood vessels. It results from relaxation of smooth muscle cells within the vessel walls, in particular in the large veins, large arteries, and smaller arterioles. The process is the opposite of vasoconstriction, which is the narrowing of blood vessels.

An arteriole is a small-diameter blood vessel in the microcirculation that extends and branches out from an artery and leads to capillaries.
Vascular resistance is the resistance that must be overcome to push blood through the circulatory system and create flow.The resistance offered by the systemic circulation is known as the systemic vascular resistance (SVR) or may sometimes be called by the older term total peripheral resistance (TPR), while the resistance offered by the pulmonary circulation is known as the pulmonary vascular resistance (PVR). Systemic vascular resistance is used in calculations of blood pressure, blood flow, and cardiac function. Vasoconstriction increases SVR, whereas vasodilation decreases SVR.
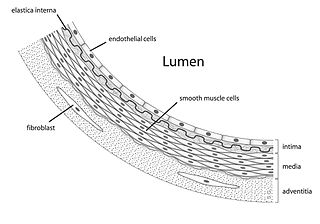
Vascular smooth muscle is the type of smooth muscle that makes up most of the walls of blood vessels.

In haemodynamics, the body must respond to physical activities, external temperature, and other factors by homeostatically adjusting its blood flow to deliver nutrients such as oxygen and glucose to stressed tissues and allow them to function. Haemodynamic response (HR) allows the rapid delivery of blood to active neuronal tissues. The brain consumes large amounts of energy but does not have a reservoir of stored energy substrates. Since higher processes in the brain occur almost constantly, cerebral blood flow is essential for the maintenance of neurons, astrocytes, and other cells of the brain. This coupling between neuronal activity and blood flow is also referred to as neurovascular coupling.

Hyperaemia is the increase of blood flow to different tissues in the body. It can have medical implications but is also a regulatory response, allowing change in blood supply to different tissues through vasodilation. Clinically, hyperaemia in tissues manifests as erythema because of the engorgement of vessels with oxygenated blood. Hyperaemia can also occur due to a fall in atmospheric pressure outside the body. The term is from Greek ὑπέρ (hupér) 'over' + αἷμα (haîma) 'blood'.
Cardiorespiratory fitness (CRF) refers to the ability of the circulatory and respiratory systems to supply oxygen to skeletal muscles during sustained physical activity. The primary measure of CRF is VO2 max. In 2016, the American Heart Association published an official scientific statement advocating that CRF be categorized as a clinical vital sign and should be routinely assessed as part of clinical practice.
The alpha-1 (α1) adrenergic receptor is a G protein-coupled receptor (GPCR) associated with the Gq heterotrimeric G-protein. It consists of three highly homologous subtypes, including α1A-, α1B-, and α1D-adrenergic. There is no α1C receptor. At one time, there was a subtype known as α1C, but it was found to be identical to the previously discovered α1A receptor subtype. To avoid confusion, naming was continued with the letter D. Catecholamines like norepinephrine (noradrenaline) and epinephrine (adrenaline) signal through the α1-adrenergic receptor in the central and peripheral nervous systems.
There are at least four known endothelin receptors, ETA, ETB1, ETB2 and ETC, all of which are G protein-coupled receptors whose activation result in elevation of intracellular-free calcium, which constricts the smooth muscles of the blood vessels, raising blood pressure, or relaxes the smooth muscles of the blood vessels, lowering blood pressure, among other functions.
Autoregulation is a process within many biological systems, resulting from an internal adaptive mechanism that works to adjust that system's response to stimuli. While most systems of the body show some degree of autoregulation, it is most clearly observed in the kidney, the heart, and the brain. Perfusion of these organs is essential for life, and through autoregulation the body can divert blood where it is most needed.
The hunting reaction or hunting response is a process of alternating vasoconstriction and vasodilation in extremities exposed to cold. The term Lewis reaction is used too, named after Thomas Lewis, who first described the effect in 1930.

Skin temperature is the temperature of the outermost surface of the body. Normal human skin temperature on the trunk of the body varies between 33.5 and 36.9 °C, though the skin's temperature is lower over protruding parts, like the nose, and higher over muscles and active organs. Recording skin temperature presents extensive difficulties. Although it is not a clear indicator of internal body temperature, skin temperature is significant in assessing the healthy function of skin. Some experts believe the physiological significance of skin temperature has been overlooked, because clinical analysis has favoured measuring temperatures of the mouth, armpit, and/or rectum. Temperatures of these parts typically are consistent with internal body temperature.
The neurovascular unit (NVU) is a group of closely related cells and extracellular matrix components that function in the homeostatic haemodynamic response of cerebral hyperaemia.
References
- 1 2 "CV Physiology | Local Regulation of Blood Flow". www.cvphysiology.com. Retrieved 2019-12-18.
- ↑ "Associate Degree Nursing Physiology Review". www.austincc.edu. Retrieved 2019-12-18.
- 1 2 3 4 5 "Local Blood Flow Regulation - Intrinsic Mechanisms". www.pathwaymedicine.org. Retrieved 2019-12-18.
- 1 2 3 4 5 6 Preston, Robin R. (2013). Physiology. Wilson, Thad E. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. ISBN 978-1-60913-241-5. OCLC 781683439.
- ↑ "Tubuloglomerular Feedback". www.pathwaymedicine.org. Retrieved 2019-12-18.
- ↑ "Pulmonary Blood Flow Regulation". www.pathwaymedicine.org. Retrieved 2019-12-18.
- ↑ "CV Physiology | Active Hyperemia". www.cvphysiology.com. Retrieved 2020-01-08.
- ↑ "CV Physiology | Reactive Hyperemia". www.cvphysiology.com. Retrieved 2020-01-08.