Related Research Articles

A brain tumor occurs when abnormal cells form within the brain. There are two main types of tumors: malignant (cancerous) tumors and benign (non-cancerous) tumors. These can be further classified as primary tumors, which start within the brain, and secondary tumors, which most commonly have spread from tumors located outside the brain, known as brain metastasis tumors. All types of brain tumors may produce symptoms that vary depending on the size of the tumor and the part of the brain that is involved. Where symptoms exist, they may include headaches, seizures, problems with vision, vomiting and mental changes. Other symptoms may include difficulty walking, speaking, with sensations, or unconsciousness.

A glioma is a type of primary tumor that starts in the glial cells of the brain or spinal cord. They are cancerous but some are extremely slow to develop. Gliomas comprise about 30 percent of all brain tumors and central nervous system tumours, and 80 percent of all malignant brain tumours.

Oligodendrogliomas are a type of glioma that are believed to originate from the oligodendrocytes of the brain or from a glial precursor cell. They occur primarily in adults but are also found in children.

Small-cell carcinoma is a type of highly malignant cancer that most commonly arises within the lung, although it can occasionally arise in other body sites, such as the cervix, prostate, and gastrointestinal tract. Compared to non-small cell carcinoma, small cell carcinoma is more aggressive, with a shorter doubling time, higher growth fraction, and earlier development of metastases.

Glioblastoma, previously known as glioblastoma multiforme (GBM), is the most aggressive and most common type of cancer that originates in the brain, and has a very poor prognosis for survival. Initial signs and symptoms of glioblastoma are nonspecific. They may include headaches, personality changes, nausea, and symptoms similar to those of a stroke. Symptoms often worsen rapidly and may progress to unconsciousness.
Bevacizumab, sold under the brand name Avastin among others, is a monoclonal antibody medication used to treat a number of types of cancers and a specific eye disease. For cancer, it is given by slow injection into a vein (intravenous) and used for colon cancer, lung cancer, ovarian cancer, glioblastoma, hepatocellular carcinoma, and renal-cell carcinoma. In many of these diseases it is used as a first-line therapy. For age-related macular degeneration it is given by injection into the eye (intravitreal).
Adjuvant therapy, also known as adjunct therapy, adjuvant care, or augmentation therapy, is a therapy that is given in addition to the primary or initial therapy to maximize its effectiveness. The surgeries and complex treatment regimens used in cancer therapy have led the term to be used mainly to describe adjuvant cancer treatments. An example of such adjuvant therapy is the additional treatment usually given after surgery where all detectable disease has been removed, but where there remains a statistical risk of relapse due to the presence of undetected disease. If known disease is left behind following surgery, then further treatment is not technically adjuvant.

PAC-1 is a synthesized chemical compound that selectively induces apoptosis, in cancerous cells. It was granted orphan drug status by the FDA in 2016.

Cilengitide is a molecule designed and synthesized at the Technical University Munich in collaboration with Merck KGaA in Darmstadt. It is based on the cyclic peptide cyclo(-RGDfV-), which is selective for αv integrins, which are important in angiogenesis, and other aspects of tumor biology. Hence, it is under investigation for the treatment of glioblastoma, where it may act by inhibiting angiogenesis, and influencing tumor invasion and proliferation.

Carmofur (INN) or HCFU (1-hexylcarbamoyl-5-fluorouracil) is a pyrimidine analogue used as an antineoplastic agent. It is a derivative of fluorouracil, being a lipophilic-masked analog of 5-FU that can be administered orally.

Olaparib, sold under the brand name Lynparza, is a medication for the maintenance treatment of BRCA-mutated advanced ovarian cancer in adults. It is a PARP inhibitor, inhibiting poly ADP ribose polymerase (PARP), an enzyme involved in DNA repair. It acts against cancers in people with hereditary BRCA1 or BRCA2 mutations, which include some ovarian, breast, and prostate cancers.
The University of Nottingham School of Pharmacy was founded in 1925 and is located in the University Park Campus of the university. The school also offers courses at the University's Malaysia campus in Kuala Lumpur with students spending two years in Malaysia and two years in Nottingham The School also offers the first joint Pharmacy course with China, with the Tianjin University of Traditional Chinese Medicine. The current head of The School is Professor Barrie Kellam (2021-).

Anaplastic astrocytoma is a rare WHO grade III type of astrocytoma, which is a type of cancer of the brain. In the United States, the annual incidence rate for anaplastic astrocytoma is 0.44 per 100,000 people.

Temozolomide, sold under the brand name Temodar among others, is an anticancer medication used to treat brain tumors such as glioblastoma and anaplastic astrocytoma. It is taken by mouth or via intravenous infusion.
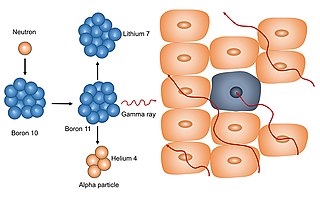
Neutron capture therapy (NCT) is a type of radiotherapy for treating locally invasive malignant tumors such as primary brain tumors, recurrent cancers of the head and neck region, and cutaneous and extracutaneous melanomas. It is a two-step process: first, the patient is injected with a tumor-localizing drug containing the stable isotope boron-10 (10B), which has a high propensity to capture low energy "thermal" neutrons. The neutron cross section of 10B is 1,000 times more than that of other elements, such as nitrogen, hydrogen, or oxygen, that occur in tissue. In the second step, the patient is radiated with epithermal neutrons, the sources of which in the past have been nuclear reactors and now are accelerators that produce higher energy epithermal neutrons. After losing energy as they penetrate tissue, the resultant low energy "thermal" neutrons are captured by the 10B atoms. The resulting decay reaction yields high-energy alpha particles that kill the cancer cells that have taken up enough 10B.
Alternating electric field therapy, sometimes called tumor treating fields (TTFields), is a type of electromagnetic field therapy using low-intensity, intermediate frequency electrical fields to treat cancer. TTFields disrupt cell division by disrupting dipole alignment and inducing dielectrophoresis of critical molecules and organelles during mitosis. These anti-mitotic effects lead to cell death, slowing cancer growth. A TTField-treatment device manufactured by the Israeli company Novocure is approved in the United States and Europe for the treatment of newly diagnosed and recurrent glioblastoma, malignant pleural mesothelioma (MPM), and is undergoing clinical trials for several other tumor types. Despite earning regulatory approval, the efficacy of this technology remains controversial among medical experts.
CUSP9 [Coordinated Undermining of Survival Paths] is one of several cancer treatment protocols using re-purposed older drugs to interfere with cancer cell's growth signaling rather than directly killing them with cytotoxic drugs. CUSP9 is a treatment specifically targeted to glioblastoma that adds to a traditional cancer cell killing drug, temozolomide, nine older, non-cytotoxic drugs to block growth factors that enhance or drive glioblastoma growth - aprepitant blocks NK-1, auranofin inhibits thioredoxin reductase, captopril inhibits angiotensin converting enzyme, celecoxib blocks cyclooxygenase-2, disulfiram blocks aldehyde dehydrogenase, itraconazole blocks Hedgehog signaling, minocycline inhibits metalloproteinase-2 and -9, quetiapine inhibits RANKL, sertraline inhibits translation-controlled tumor protein [TCTP]. These targets have been shown to be active in promoting glioblastoma growth.
Elizabeth Ruth Plummer is a Professor of Experimental Cancer Medicine at Newcastle University and an oncologist specialising in treating patients with melanoma. Based in Newcastle, she directs the Sir Bobby Robson Cancer Trials Research Centre, set up by the Sir Bobby Robson Foundation to run early-stage clinical trials.v Plummer and the Newcastle team won a 2010 Translational Cancer Research Prize from Cancer Research UK for work using rucaparib to treat ovarian cancer. Plummer was elected as a fellow of the UK's Academy of Medical Sciences in 2018.
John A. Hickman is a British-French cancer pharmacologist.
Henry Brem, M.D. is an American neurosurgeon, researcher, educator and inventor known for introducing an image guidance computer system to deliver targeted chemotherapy to intraoperative brain tumors. As of 2023, he is the Harvey Cushing Professor, Director of the Department of Neurosurgery, Professor of Neurosurgery, Ophthalmology, Oncology and Biomedical Engineering Neurosurgeon-in-Chief, and Director, Hunterian Neurosurgical Research Center and Director at Johns Hopkins in Baltimore, Maryland. Brem has written more than 490 peer-reviewed articles, 50 books and book chapters and holds 11 patents.
References
- 1 2 "Malcolm Stevens". The Royal Society. Retrieved 5 September 2017.
- 1 2 "Malcolm Stevens". School of Pharmacy. University of Nottingham. Retrieved 5 September 2017.
- ↑ "100 Inspiring Minds – Professor Malcolm Stevens OBE, FRS". Bolton School. Archived from the original on 6 September 2017. Retrieved 5 September 2017.
- ↑ "Marriage index entry". FreeBMD. ONS. September 1961. Retrieved 6 September 2017.
- ↑ "Marriage Indexes". lancashirebmd.org.uk. Retrieved 6 September 2017.
- ↑ "Professor Malcolm Stevens OBE, FRS". 50 Aston Greats. Aston University. Retrieved 5 September 2017.
- ↑ Weller, Michael; et al. (17 June 2019). "How we treat glioblastoma". ESMO Open. 4 (Suppl 2): e000520. doi:10.1136/esmoopen-2019-000520. PMC 6586206 . PMID 31297242.
- ↑ Stupp, Roger; et al. (10 March 2005). "Radiotherapy plus Concomitant and Adjuvant Temozolomide for Glioblastoma". New England Journal of Medicine. 352 (10): 987–996. doi: 10.1056/NEJMoa043330 . PMID 15758009.
- ↑ "No. 55354". The London Gazette (Supplement). 31 December 1998. p. 13.