Urinary incontinence (UI), also known as involuntary urination, is any uncontrolled leakage of urine. It is a common and distressing problem, which may have a large impact on quality of life. It has been identified as an important issue in geriatric health care. The term enuresis is often used to refer to urinary incontinence primarily in children, such as nocturnal enuresis. UI is an example of a stigmatized medical condition, which creates barriers to successful management and makes the problem worse. People may be too embarrassed to seek medical help, and attempt to self-manage the symptom in secrecy from others.

Fecal incontinence (FI), or in some forms, encopresis, is a lack of control over defecation, leading to involuntary loss of bowel contents, both liquid stool elements and mucus, or solid feces. When this loss includes flatus (gas), it is referred to as anal incontinence. FI is a sign or a symptom, not a diagnosis. Incontinence can result from different causes and might occur with either constipation or diarrhea. Continence is maintained by several interrelated factors, including the anal sampling mechanism, and incontinence usually results from a deficiency of multiple mechanisms. The most common causes are thought to be immediate or delayed damage from childbirth, complications from prior anorectal surgery, altered bowel habits. An estimated 2.2% of community-dwelling adults are affected. However, reported prevalence figures vary. A prevalence of 8.39% among non-institutionalized U.S adults between 2005 and 2010 has been reported, and among institutionalized elders figures come close to 50%.

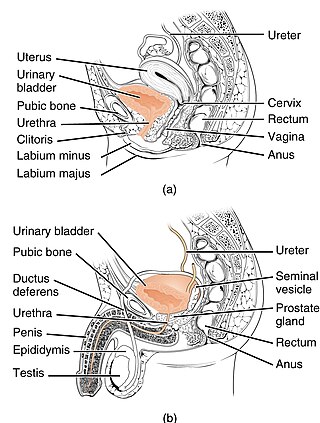
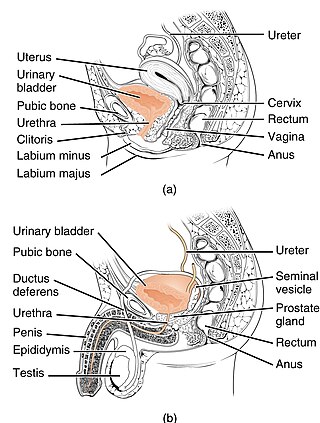
In urinary catheterization, a latex, polyurethane, or silicone tube known as a urinary catheter is inserted into the bladder through the urethra to allow urine to drain from the bladder for collection. It may also be used to inject liquids used for treatment or diagnosis of bladder conditions. A clinician, often a nurse, usually performs the procedure, but self-catheterization is also possible. A catheter may be in place for long periods of time or removed after each use.
In anatomy, a stoma is any opening in the body. For example, a mouth, a nose, and an anus are natural stomata. Any hollow organ can be manipulated into an artificial stoma as necessary. This includes the esophagus, stomach, duodenum, ileum, colon, pleural cavity, ureters, urinary bladder, and renal pelvis. Such a stoma may be permanent or temporary.

Prostatectomy is the surgical removal of all or part of the prostate gland. This operation is done for benign conditions that cause urinary retention, as well as for prostate cancer and for other cancers of the pelvis.

A nephrostomy or percutaneous nephrostomy is an artificial opening created between the kidney and the skin which allows for the urinary diversion directly from the upper part of the urinary system. It is an interventional radiology/surgical procedure in which the renal pelvis is punctured whilst using imaging as guidance. Images are obtained once an antegrade pyelogram, with a fine needle, has been performed. A nephrostomy tube may then be placed to allow drainage.

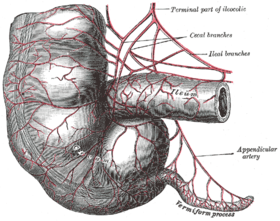
The Mitrofanoff procedure, also known as the Mitrofanoff appendicovesicostomy, is a surgical procedure in which the appendix is used to create a conduit, or channel, between the skin surface and the urinary bladder. The small opening on the skin surface, or the stoma, is typically located either in the navel or nearby the navel on the right lower side of the abdomen. Originally developed by Professor Paul Mitrofanoff in 1980, the procedure represents an alternative to urethral catheterization and is sometimes used by people with urethral damage or by those with severe autonomic dysreflexia. An intermittent catheter, or a catheter that is inserted and then removed after use, is typically passed through the channel every 3–4 hours and the urine is drained into a toilet or a bottle. As the bladder fills, rising pressure compresses the channel against the bladder wall, creating a one-way valve that prevents leakage of urine between catheterizations.

Radical retropubic prostatectomy is a surgical procedure in which the prostate gland is removed through an incision in the abdomen. It is most often used to treat individuals who have early prostate cancer. Radical retropubic prostatectomy can be performed under general, spinal, or epidural anesthesia and requires blood transfusion less than one-fifth of the time. Radical retropubic prostatectomy is associated with complications such as urinary incontinence and impotence, but these outcomes are related to a combination of individual patient anatomy, surgical technique, and the experience and skill of the surgeon.
Percutaneous tibial nerve stimulation (PTNS), also referred to as posterior tibial nerve stimulation, is the least invasive form of neuromodulation used to treat overactive bladder (OAB) and the associated symptoms of urinary urgency, urinary frequency and urge incontinence. These urinary symptoms may also occur with interstitial cystitis and following a radical prostatectomy. Outside the United States, PTNS is also used to treat fecal incontinence.
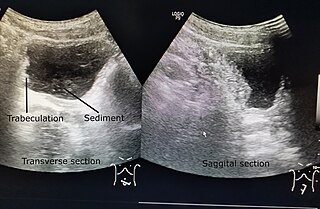
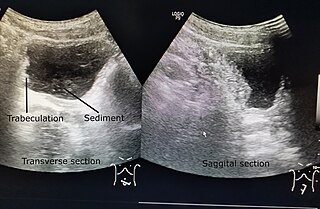
Neurogenic bladder dysfunction, often called by the shortened term neurogenic bladder, refers to urinary bladder problems due to disease or injury of the central nervous system or peripheral nerves involved in the control of urination. There are multiple types of neurogenic bladder depending on the underlying cause and the symptoms. Symptoms include overactive bladder, urinary urgency, frequency, incontinence or difficulty passing urine. A range of diseases or conditions can cause neurogenic bladder including spinal cord injury, multiple sclerosis, stroke, brain injury, spina bifida, peripheral nerve damage, Parkinson's disease, multiple system atrophy or other neurodegenerative diseases. Neurogenic bladder can be diagnosed through a history and physical as well as imaging and more specialized testing. In addition to symptomatic treatment, treatment depends on the nature of the underlying disease and can be managed with behavioral changes, medications, surgeries, or other procedures. The symptoms of neurogenic bladder, especially incontinence, can severely degrade a person's quality of life.

Overactive bladder (OAB) is a common condition where there is a frequent feeling of needing to urinate to a degree that it negatively affects a person's life. The frequent need to urinate may occur during the day, at night, or both. Loss of bladder control may occur with this condition. This condition is also sometimes characterized by a sudden and involuntary contraction of the bladder muscles, in response to excitement or anticipation. This in turn leads to a frequent and urgent need to urinate.
Sacral nerve stimulation, also termed sacral neuromodulation, is a type of medical electrical stimulation therapy.
The Monti procedure is a surgical procedure in which a part of the gastrointestinal tract is used to create a continent conduit between the skin surface and the urinary bladder or a neobladder.
In urology, the Mitrofanoff principle is the creation of a passageway for urine or enema fluid that, by its (surgical) construction, has a valve mechanism to allow continence.
Bowel management is the process which a person with a bowel disability uses to manage fecal incontinence or constipation. People who have a medical condition which impairs control of their defecation use bowel management techniques to choose a predictable time and place to evacuate. A simple bowel management technique might include diet control and establishing a toilet routine. As a more involved practice a person might use an enema to relieve themselves. Without bowel management, the person might either suffer from the feeling of not getting relief, or they might soil themselves.
Urogynecology or urogynaecology is a surgical sub-specialty of urology and gynecology.
In fecal incontinence (FI), surgery may be carried out if conservative measures alone are not sufficient to control symptoms. There are many surgical options described for FI, and they can be considered in 4 general groups.

An artificial urinary sphincter (AUS) is an implanted device to treat moderate to severe stress urinary incontinence, most commonly in men. The AUS is designed to supplement the function of the natural urinary sphincter that restricts urine flow out of the bladder.
Transanal irrigation of the rectum and colon is designed to assist the evacuation of feces from the bowel by introducing water into these compartments via the anus.

If medical treatment is not effective, surgery may need to be performed for benign prostatic hyperplasia.