Related Research Articles

Hildegard E. Peplau was an American nurse and the first published nursing theorist since Florence Nightingale. She created the middle-range nursing theory of interpersonal relations, which helped to revolutionize the scholarly work of nurses. As a primary contributor to mental health law reform, she led the way towards humane treatment of patients with behavior and personality disorders.
Nursing theory is defined as "a creative and conscientious structuring of ideas that project a tentative, purposeful, and systematic view of phenomena". Through systematic inquiry, whether in nursing research or practice, nurses are able to develop knowledge relevant to improving the care of patients. Theory refers to "a coherent group of general propositions used as principles of explanation".

Pediatric nursing is part of the nursing profession, specifically revolving around the care of neonates and children up to adolescence. The word, pediatrics, comes from the Greek words 'paedia' (child) and 'iatrike' (physician). 'Paediatrics' is the British/Australian spelling, while 'pediatrics' is the American spelling.
Psychiatric nursing or mental health nursing is the appointed position of a nurse that specialises in mental health, and cares for people of all ages experiencing mental illnesses or distress. These include: neurodevelopmental disorders, schizophrenia, schizoaffective disorder, mood disorders, addiction, anxiety disorders, personality disorders, eating disorders, suicidal thoughts, psychosis, paranoia, and self-harm.

A nurse practitioner (NP) is an advanced practice registered nurse and a type of mid-level practitioner. NPs are trained to assess patient needs, order and interpret diagnostic and laboratory tests, diagnose disease, prescribe medications and formulate treatment plans. NP training covers basic disease prevention, coordination of care, and health promotion.
Home health is a nursing specialty in which nurses provide multidimensional home care to patients of all ages. Home health care is a cost efficient way to deliver quality care in the convenience of the client's home. Home health nurses create care plans to achieve goals based on the client's diagnosis. These plans can include preventive, therapeutic, and rehabilitative actions. Home health nurses also supervise certified nursing assistants. The professional nursing organization for home health nurses is the Home Healthcare Nurses Association (HHNA). Home health care is intended for clients that are well enough to be discharged home, but still require skilled nursing personnel to assess, initiate and oversee nursing interventions.
Primary nursing is a system of nursing care delivery that emphasizes continuity of care and responsibility acceptance by having one registered nurse (RN), often teamed with a licensed practical nurse (LPN) and/or nursing assistant (NA), who together provide complete care for a group of patients throughout their stay in a hospital unit or department. While the patient is on the nurses' unit, the primary nurse accepts responsibility for administering some and coordinating all aspects of the patient's nursing care, with the support of other members of the nursing staff. This results in the nurse having greater insight into the patient's condition, both medical and emotional.

Nursing in the United States is a professional health care occupation. It is the largest such occupation, employing millions of certified professionals. As of 2023, 3,175,390 registered nurses were employed, paid a median income of $86,070.
Georgetown UniversitySchool of Nursing is one of the eleven schools of Georgetown University. Founded in 1903 as the School of Nursing, it added three other health related majors in 1999 and appended its name to become the School of Nursing & Health Studies. In 2022, the school returned to the name School of Nursing, as the School of Health was divided from it. The school has been at the forefront of education in the health care field, offering many programs unique to America's elite institutions. Offering undergraduate and graduate programs in the health sciences, graduates are prepared to enter the complex fields of medicine, law, health policy, and nursing. The School of Nursing is made up of the Department of Health Systems Administration, the Department of Human Science, the Department of International Health, and the Department of Nursing.
Health administration, healthcare administration, healthcare management or hospitalmanagement is the field relating to leadership, management, and administration of public health systems, health care systems, hospitals, and hospital networks in all the primary, secondary, and tertiary sectors.

Nursing is a health care profession that "integrates the art and science of caring and focuses on the protection, promotion, and optimization of health and human functioning; prevention of illness and injury; facilitation of healing; and alleviation of suffering through compassionate presence". Nurses practice in many specialties with varying levels of certification and responsibility. Nurses comprise the largest component of most healthcare environments. There are shortages of qualified nurses in many countries.
The healthcare error proliferation model is an adaptation of James Reason’s Swiss Cheese Model designed to illustrate the complexity inherent in the contemporary healthcare delivery system and the attribution of human error within these systems. The healthcare error proliferation model explains the etiology of error and the sequence of events typically leading to adverse outcomes. This model emphasizes the role organizational and external cultures contribute to error identification, prevention, mitigation, and defense construction.
Integrated care, also known as integrated health, coordinated care, comprehensive care, seamless care, interprofessional care or transmural care, is a worldwide trend in health care reforms and new organizational arrangements focusing on more coordinated and integrated forms of care provision. Integrated care may be seen as a response to the fragmented delivery of health and social services being an acknowledged problem in many health systems. This model of care is working towards moving away from a siloed and referral-based format of care to a team-based model.

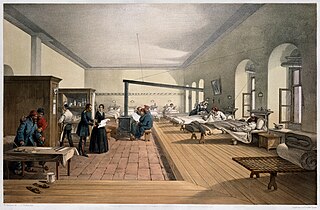
The history of nursing in the United States focuses on the professionalization of Nursing in the United States since the Civil War.
Creative Health Care Management (CHCM) is a private U.S. corporation, which provides consultation and training in the health care sector. CHCM is based in Bloomington, Minnesota. Founded in 1982 by Marie Manthey, it was originally called Creative Nursing Management. The name change to CHCM was in recognition of the systemic nature of change.

The Minneapolis Veterans Affairs Health Care System (VAHCS) is network of hospital and outpatient clinics based in Minneapolis, Minnesota, USA. It belongs to the VISN23 VA Midwest Health Care Network managed by the Veterans Health Administration of the Department of Veterans Affairs. The Minneapolis VAHCS provides healthcare for United States military veterans in areas such as medicine, surgery, psychiatry, physical medicine and rehabilitation, neurology, oncology, dentistry, geriatrics and extended care. As a teaching hospital, it operates comprehensive training programs for multiple treatment specialties. The Minneapolis VAHCS also hosts one of the largest research programs of any VA health care system and maintains research affiliations with the University of Minnesota.

Helga Jónsdóttir is a professor in nursing at the Faculty of Nursing in the School of Health Sciences at the University of Iceland and Academic Chair of Nursing Care for Chronically Ill Adults in a joint position at Landspítali the National University Hospital.

Elizabeth June Werner was an American nursing executive and educator. She was chair of the department of nursing for 19 years at Evanston Hospital, Illinois, and retired in 1990 as chairperson emerita. During this period she launched the nation's first primary nursing model, transforming the relationship between patients and their caregivers. She also formalized mentoring and professionalized the nursing staff.

Frances Mary McHie Rains (1911–2006) was an American nurse. She was the first Black woman admitted to the University of Minnesota School of Nursing. She was admitted to the School of Nursing after the Minnesota State Legislature learned of her initial rejection from the school based on race. She graduated in 1932.

Wilton Sebastian Kezala Wakooli is a Ugandan professor, academic administrator, medical educationist, researcher, and nurse. He co-founded the International Institute of Health Sciences (IIHS), Uganda in 1998. He served as chairman for the Uganda Nurses and Midwives Examinations Board (UNMEB). He is a co-founder and former chairman of the Uganda Private Health Training Insitutions Association (UPHTIA). He is a former secretary general for The Aids Support Organization (TASO) Uganda and also Busoga Kingdom. He is the executive director of the International Institute of Health Sciences (IIHS). He served also served as a Consultant for the World Health Organization (WHO) at Cuttington University College (CUC) in the Division of Nursing.
References
- ↑ "Academy Living Legends". American Academy of Nursing . Retrieved 13 December 2017.
- ↑ Tobbell, Dominique A, PhD (2010). "Marie Manthey Interview - Academic Health Center Oral History Project" University of Minnesota. 2010. P 3-7
- 1 2 Silberg, Barbara (2002). "The Human Face of Health Care" MINNESOTA: The Magazine of the University of Minnesota Alumni Association. March/April 2002. P 33
- 1 2 Manthey, Marie (1999). "I Never Saw Myself as a Change Agent". Reflections. Vol. 25, no. 2. Sigma Theta Tau nursing honor society. pp. 19–21. ISSN 0885-8144.
- 1 2 3 Williams, Sarah T (2014). "One Woman's Effort to Understand the Problem of Nursing and Addiction." MinnPost. 5/28/14
- 1 2 3 Villaire, Michael (1993) Marie Manthey interview on Evolution of Primary Nursing.
- ↑ Zyda, Joan (1978) Chicago Tribune.
- ↑ Manthey, Marie (1999). "Financial Management for Entrepreneurs" Nursing Administration Quarterly, by Aspen Publication. Summer 1999. P 81-82. Vol. 23, No 4 J0392. ISSN 0363-9568
- ↑ 'The Application of Primary Nursing in a Hospital Setting,' a Study by the U.S. Department of Health and Human Services, 1983. p iv.
- ↑ Manthey, Marie (2013) Foreword: Advancing Professional Nursing Practice.
- Zyda, Joan (1978) 'Primary Nursing - Hospitals bring back Florence Nightingale.' Chicago Tribune (Lifestyle, Sec 5). 2/26/78.
- "The Application of Primary Nursing in a Hospital Setting" (1983). U.S. Department of Health and Human Services, Public Health Service, Health Resources and Services Administration. DHHS Publication No. HRS-P-DN-83-1.
- Villaire, Michael (1993). Interview: Marie Manthey on the Evolution of Primary Nursing. Critical Care Nurse December 1993. pp 100–107. ISSN 0279-5442
- Kalstrom, Jonathan (1994). "Nursing: It's Your Business." Minnesota Nurse Magazine Vol I, # 15, Jan 1994. pp 8–12.
- Tyler, Kate (1999). "School of Nursing Alumnae: Marie Manthey, Pathbreaking Visionary." Network [Published by the University of Minnesota School of Nursing] Vol 1, No 1. Spring/Summer 1999. pp 16–17.
- Silberg, Barbara (2002). "The Human Face of Health Care: The University's School of Nursing is a Leader in Preparing Future Nurses for the Challenges of Practice and the Delivery of Patient Care - From Addressing Workplace Issues to Applying Research Aimed at Improving the Health of People Around the World." MINNESOTA: The Magazine of the University of Minnesota Alumni Association. March/April 2002. pp 28–35.
- Williams, Sarah T (2014). "One Woman's Effort to Understand the Problem of Nursing and Addiction." MinnPost. 5/28/14.
- Steiner, Andy (2017). "New Curriculum Brings Clear-Eyed Focus to Substance-Use Disorder in Nursing." MinnPost. 4/12/17.