Related Research Articles

A bone is a rigid organ that constitutes part of the skeleton in most vertebrate animals. Bones protect the various other organs of the body, produce red and white blood cells, store minerals, provide structure and support for the body, and enable mobility. Bones come in a variety of shapes and sizes and have complex internal and external structures. They are lightweight yet strong and hard and serve multiple functions.

Osteoporosis is a systemic skeletal disorder characterized by low bone mass, micro-architectural deterioration of bone tissue leading to bone sterility, and consequent increase in fracture risk. It is the most common reason for a broken bone among the elderly. Bones that commonly break include the vertebrae in the spine, the bones of the forearm, the wrist, and the hip. Until a broken bone occurs there are typically no symptoms. Bones may weaken to such a degree that a break may occur with minor stress or spontaneously. After the broken bone heals, the person may have chronic pain and a decreased ability to carry out normal activities.

Bisphosphonates are a class of drugs that prevent the loss of bone density, used to treat osteoporosis and similar diseases. They are the most commonly prescribed drugs used to treat osteoporosis. They are called bisphosphonates because they have two phosphonate groups. They are thus also called diphosphonates.

Paget's disease of bone is a condition involving cellular remodeling and deformity of one or more bones. The affected bones show signs of dysregulated bone remodeling at the microscopic level, specifically excessive bone breakdown and subsequent disorganized new bone formation. These structural changes cause the bone to weaken, which may result in deformity, pain, fracture or arthritis of associated joints.

Fibrous dysplasia is a disorder where normal bone and marrow is replaced with fibrous tissue, resulting in formation of bone that is weak and prone to expansion. As a result, most complications result from fracture, deformity, functional impairment, and pain. Disease occurs along a broad clinical spectrum ranging from asymptomatic, incidental lesions, to severe disabling disease. Disease can affect one bone (monostotic), multiple (polyostotic), or all bones (panostotic) and may occur in isolation or in combination with café au lait skin macules and hyperfunctioning endocrinopathies, termed McCune–Albright syndrome. More rarely, fibrous dysplasia may be associated with intramuscular myxomas, termed Mazabraud's syndrome. Fibrous dysplasia is very rare, and there is no known cure. Fibrous dysplasia is not a form of cancer.

Osteopenia, known as "low bone mass" or "low bone density", is a condition in which bone mineral density is low. Because their bones are weaker, people with osteopenia may have a higher risk of fractures, and some people may go on to develop osteoporosis. In 2010, 43 million older adults in the US had osteopenia. Unlike osteoporosis, osteopenia does not usually cause symptoms, and losing bone density in itself does not cause pain.

Sclerostin is a protein that in humans is encoded by the SOST gene. It is a secreted glycoprotein with a C-terminal cysteine knot-like (CTCK) domain and sequence similarity to the DAN family of bone morphogenetic protein (BMP) antagonists. Sclerostin is produced primarily by the osteocyte but is also expressed in other tissues, and has anti-anabolic effects on bone formation.

Bone density, or bone mineral density, is the amount of bone mineral in bone tissue. The concept is of mass of mineral per volume of bone, although clinically it is measured by proxy according to optical density per square centimetre of bone surface upon imaging. Bone density measurement is used in clinical medicine as an indirect indicator of osteoporosis and fracture risk. It is measured by a procedure called densitometry, often performed in the radiology or nuclear medicine departments of hospitals or clinics. The measurement is painless and non-invasive and involves low radiation exposure. Measurements are most commonly made over the lumbar spine and over the upper part of the hip. The forearm may be scanned if the hip and lumbar spine are not accessible.

Quantitative computed tomography (QCT) is a medical technique that measures bone mineral density (BMD) using a standard X-ray Computed Tomography (CT) scanner with a calibration standard to convert Hounsfield Units (HU) of the CT image to bone mineral density values. Quantitative CT scans are primarily used to evaluate bone mineral density at the lumbar spine and hip.

Ibandronic acid is a bisphosphonate medication used in the prevention and treatment of osteoporosis and metastasis-associated skeletal fractures in people with cancer. It may also be used to treat hypercalcemia. It is typically formulated as its sodium salt ibandronate sodium.
Senile osteoporosis has been recently recognized as a geriatric syndrome with a particular pathophysiology. There are different classification of osteoporosis: primary, in which bone loss is a result of aging and secondary, in which bone loss occurs from various clinical and lifestyle factors. Primary, or involuntary osteoporosis, can further be classified into Type I or Type II. Type I refers to postmenopausal osteoporosis and is caused by the deficiency of estrogen. While senile osteoporosis is categorized as an involuntary, Type II, and primary osteoporosis, which affects both men and women over the age of 70 years. It is accompanied by vitamin D deficiency, body's failure to absorb calcium, and increased parathyroid hormone.
Steroid-induced osteoporosis is osteoporosis arising from the use of glucocorticoids analogous to Cushing's syndrome but involving mainly the axial skeleton. The synthetic glucocorticoid prescription drug prednisone is a main candidate after prolonged intake. Bisphosphonates are beneficial in reducing the risk of vertebral fractures. Some professional guidelines recommend prophylactic calcium and vitamin D supplementation in patients who take the equivalent of more than 30 mg hydrocortisone, especially when this is in excess of three months. The use of thiazide diuretics, and gonadal hormone replacement has also been recommended, with the use of calcitonin, bisphosphonates, sodium fluoride or anabolic steroids also suggested in refractory cases. Alternate day use may not prevent this complication.
FRAX is a diagnostic tool used to evaluate the 10-year probability of bone fracture risk. It was developed by the University of Sheffield. FRAX integrates clinical risk factors and bone mineral density at the femoral neck to calculate the 10-year probability of hip fracture and the 10-year probability of a major osteoporotic fracture. The models used to develop the FRAX diagnostic tool were derived from studying patient populations in North America, Europe, Latin America, Asia and Australia.
Abaloparatide, sold under the brand name Tymlos among others, is a parathyroid hormone-related protein (PTHrP) analog medication used to treat osteoporosis. It is an anabolic agent.
The trabecular bone score is a measure of bone texture correlated with bone microarchitecture and a marker for the risk of osteoporosis. Introduced in 2008, its main projected use is alongside measures of bone density in better predicting fracture risk in people with metabolic bone problems.
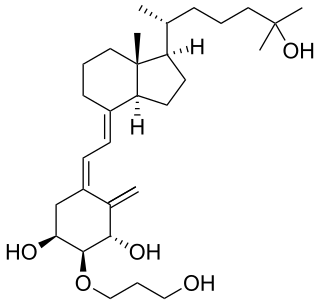
Eldecalcitol is an analog of calcitriol, the active form of vitamin D.
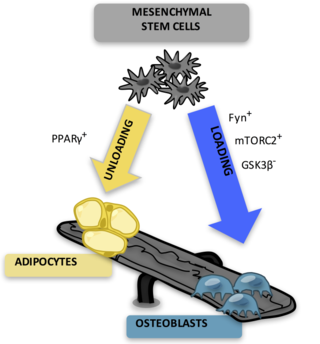
Bone marrow adipose tissue (BMAT), sometimes referred to as marrow adipose tissue (MAT), is a type of fat deposit in bone marrow. It increases in states of low bone density -osteoporosis, anorexia nervosa/ caloric restriction, skeletal unweighting such as that which occurs in space travel, and anti-diabetes therapies. BMAT decreases in anaemia, leukaemia, and hypertensive heart failure; in response to hormones such as oestrogen, leptin, and growth hormone; with exercise-induced weight loss or bariatric surgery; in response to chronic cold exposure; and in response to pharmacological agents such as bisphosphonates, teriparatide, and metformin.
Single photon absorptiometry is a measuring method for bone density invented by John R. Cameron and James A. Sorenson in 1963.
A bone biopsy is a procedure in which a small bone sample is removed from the outer layers of bone for examination, unlike a bone marrow biopsy, which involves the innermost part of the bone. The bone biopsy sample retains the architecture of bone when seen using histopathological examination slide.
Judith Elizabeth Adams was an English professor, musculoskeletal radiologist, honorary consultant, and clinical director of the radiology department at Manchester University NHS Foundation Trust.
References
- ↑ Rapp, Goldie (2018-09-11). "From PHS to a career at MIT and Harvard". Shaw Local. Retrieved 2023-06-01.
- 1 2 "Bouxsein Lab | Lab Members".
- ↑ Carter, Dennis R.; Bouxsein, Mary L.; Marcus, Robert (2009-12-03). "New approaches for interpreting projected bone densitometry data". Journal of Bone and Mineral Research. 7 (2): 137–145. doi:10.1002/jbmr.5650070204. PMID 1570758. S2CID 1843926.
- ↑ Bouxsein, M. L.; Radloff, S. E. (1997-05-01). "Quantitative Ultrasound of the Calcaneus Reflects the Mechanical Properties of Calcaneal Trabecular Bone". Journal of Bone and Mineral Research. 12 (5): 839–846. doi: 10.1359/jbmr.1997.12.5.839 . PMID 9144351.
- ↑ Bouxsein, Mary L; Boyd, Stephen K; Christiansen, Blaine A; Guldberg, Robert E; Jepsen, Karl J; Müller, Ralph (2010-06-07). "Guidelines for assessment of bone microstructure in rodents using micro-computed tomography". Journal of Bone and Mineral Research. 25 (7): 1468–1486. doi: 10.1002/jbmr.141 . PMID 20533309.
- ↑ Rosen, Clifford J; Bouxsein, Mary L (2006). "Mechanisms of Disease: is osteoporosis the obesity of bone?". Nature Clinical Practice Rheumatology. 2 (1): 35–43. doi:10.1038/ncprheum0070. ISSN 1745-8382. PMID 16932650. S2CID 9953651.
- ↑ Burkhart, Katelyn; Allaire, Brett; Bouxsein, Mary L. (2019-06-15). "Negative Effects of Long-duration Spaceflight on Paraspinal Muscle Morphology". Spine. 44 (12): 879–886. doi:10.1097/BRS.0000000000002959. ISSN 0362-2436. PMID 30624302. S2CID 58537896.
- ↑ Popp, Kristin L.; Ackerman, Kathryn E.; Rudolph, Sara E.; Johannesdottir, Fjola; Hughes, Julie M.; Tenforde, Adam S.; Bredella, Miriam A.; Xu, Chun; Unnikrishnan, Ginu; Reifman, Jaques; Bouxsein, Mary L. (2021). "Changes in Volumetric Bone Mineral Density Over 12 Months After a Tibial Bone Stress Injury Diagnosis: Implications for Return to Sports and Military Duty". The American Journal of Sports Medicine. 49 (1): 226–235. doi:10.1177/0363546520971782. ISSN 0363-5465. PMID 33259223. S2CID 227251698.
- ↑ "Mary Bouxsein Mary Larsen Bouxsein, Ph.D. To be Inducted into Medical and Biological Engineering Elite - AIMBE". March 5, 2015. Retrieved 2023-06-01.