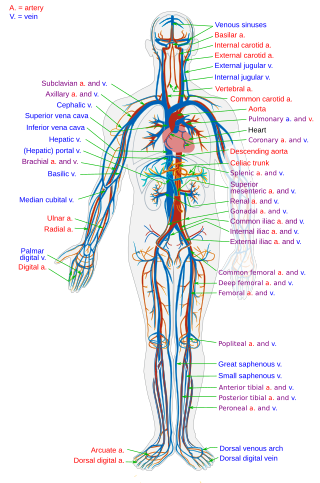
Veins are blood vessels in the circulatory system of humans and most other animals that carry blood towards the heart. Most veins carry deoxygenated blood from the tissues back to the heart; exceptions are those of the pulmonary and fetal circulations which carry oxygenated blood to the heart. In the systemic circulation, arteries carry oxygenated blood away from the heart, and veins return deoxygenated blood to the heart, in the deep veins.

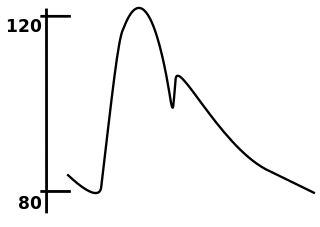
Blood pressure (BP) is the pressure of circulating blood against the walls of blood vessels. Most of this pressure results from the heart pumping blood through the circulatory system. When used without qualification, the term "blood pressure" refers to the pressure in a brachial artery, where it is most commonly measured. Blood pressure is usually expressed in terms of the systolic pressure over diastolic pressure in the cardiac cycle. It is measured in millimeters of mercury (mmHg) above the surrounding atmospheric pressure, or in kilopascals (kPa). The difference between the systolic and diastolic pressures is known as pulse pressure, while the average pressure during a cardiac cycle is known as mean arterial pressure.
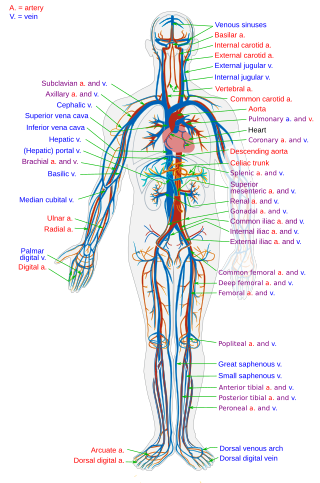
The circulatory system is a system of organs that includes the heart, blood vessels, and blood which is circulated throughout the entire body of a human or other vertebrate. It includes the cardiovascular system, or vascular system, that consists of the heart and blood vessels. The circulatory system has two divisions, a systemic circulation or circuit, and a pulmonary circulation or circuit. Some sources use the terms cardiovascular system and vascular system interchangeably with circulatory system.
Baroreceptors are sensors located in the carotid sinus and in the aortic arch. They sense the blood pressure and relay the information to the brain, so that a proper blood pressure can be maintained.

In cardiac physiology, cardiac output (CO), also known as heart output and often denoted by the symbols , , or , is the volumetric flow rate of the heart's pumping output: that is, the volume of blood being pumped by a single ventricle of the heart, per unit time. Cardiac output (CO) is the product of the heart rate (HR), i.e. the number of heartbeats per minute (bpm), and the stroke volume (SV), which is the volume of blood pumped from the left ventricle per beat; thus giving the formula:
Hemodynamics or haemodynamics are the dynamics of blood flow. The circulatory system is controlled by homeostatic mechanisms of autoregulation, just as hydraulic circuits are controlled by control systems. The hemodynamic response continuously monitors and adjusts to conditions in the body and its environment. Hemodynamics explains the physical laws that govern the flow of blood in the blood vessels.
In cardiovascular physiology, stroke volume (SV) is the volume of blood pumped from the ventricle per beat. Stroke volume is calculated using measurements of ventricle volumes from an echocardiogram and subtracting the volume of the blood in the ventricle at the end of a beat from the volume of blood just prior to the beat. The term stroke volume can apply to each of the two ventricles of the heart, although when not explicitly stated it refers to the left ventricle and should therefore be referred to as left stroke volume (LSV). The stroke volumes for each ventricle are generally equal, both being approximately 90 mL in a healthy 70-kg man. Any persistent difference between the two stroke volumes, no matter how small, would inevitably lead to venous congestion of and/or shunt between the systemic and the pulmonary circulation.
A cardiac function curve is a graph showing the relationship between right atrial pressure (x-axis) and cardiac output (y-axis). Superimposition of the cardiac function curve and venous return curve is used in one hemodynamic model.

Mitral stenosis is a valvular heart disease characterized by the narrowing of the opening of the mitral valve of the heart. It is almost always caused by rheumatic valvular heart disease. Normally, the mitral valve is about 5 cm2 during diastole. Any decrease in area below 2 cm2 causes mitral stenosis. Early diagnosis of mitral stenosis in pregnancy is very important as the heart cannot tolerate increased cardiac output demand as in the case of exercise and pregnancy. Atrial fibrillation is a common complication of resulting left atrial enlargement, which can lead to systemic thromboembolic complications such as stroke.

Atrial septal defect (ASD) is a congenital heart defect in which blood flows between the atria of the heart. Some flow is a normal condition both pre-birth and immediately post-birth via the foramen ovale; however, when this does not naturally close after birth it is referred to as a patent (open) foramen ovale (PFO). It is common in patients with a congenital atrial septal aneurysm (ASA).
Vascular resistance is the resistance that must be overcome for blood to flow through the circulatory system. The resistance offered by the systemic circulation is known as the systemic vascular resistance (SVR) or may sometimes be called by the older term total peripheral resistance (TPR), while the resistance offered by the pulmonary circulation is known as the pulmonary vascular resistance (PVR). Systemic vascular resistance is used in calculations of blood pressure, blood flow, and cardiac function. Vasoconstriction increases SVR, whereas vasodilation decreases SVR.

The jugular venous pressure is the indirectly observed pressure over the venous system via visualization of the internal jugular vein. It can be useful in the differentiation of different forms of heart and lung disease. Classically three upward deflections and two downward deflections have been described.
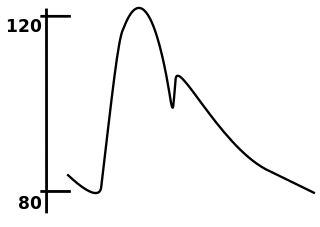
In medicine, the mean arterial pressure (MAP) is an average calculated blood pressure in an individual during a single cardiac cycle. Although methods of estimating MAP vary, a common calculation is to take one-third of the pulse pressure, and add that amount to the diastolic pressure. A normal MAP is about 90 mmHg.

The cardiac cycle is the performance of the human heart from the beginning of one heartbeat to the beginning of the next. It consists of two periods: one during which the heart muscle relaxes and refills with blood, called diastole, following a period of robust contraction and pumping of blood, called systole. After emptying, the heart relaxes and expands to receive another influx of blood returning from the lungs and other systems of the body, before again contracting to pump blood to the lungs and those systems.

Central venous pressure (CVP) is the blood pressure in the venae cavae, near the right atrium of the heart. CVP reflects the amount of blood returning to the heart and the ability of the heart to pump the blood back into the arterial system. CVP is often a good approximation of right atrial pressure (RAP), although the two terms are not identical, as a pressure differential can sometimes exist between the venae cavae and the right atrium. CVP and RAP can differ when arterial tone is altered. This can be graphically depicted as changes in the slope of the venous return plotted against right atrial pressure.
A cardiac shunt is a pattern of blood flow in the heart that deviates from the normal circuit of the circulatory system. It may be described as right-left, left-right or bidirectional, or as systemic-to-pulmonary or pulmonary-to-systemic. The direction may be controlled by left and/or right heart pressure, a biological or artificial heart valve or both. The presence of a shunt may also affect left and/or right heart pressure either beneficially or detrimentally.

Etilefrine is a cardiac stimulant used as an antihypotensive. It is a sympathomimetic amine of the 3-hydroxy-phenylethanolamine series used in treating orthostatic hypotension of neurological, cardiovascular, endocrine or metabolic origin. Intravenous infusion of this compound increases cardiac output, stroke volume, venous return and blood pressure in man and experimental animals, suggesting stimulation of both α and β adrenergic receptors. However, in vitro studies indicate that etilefrine has a much higher affinity for β1 (cardiac) than for β2 adrenoreceptors.
Venous return is the rate of blood flow back to the heart. It normally limits cardiac output.
Low pressure baroreceptors are baroreceptors that relay information derived from blood pressure within the autonomic nervous system. They are stimulated by stretching of the vessel wall. They are located in large systemic veins and in the walls of the atria of the heart, and pulmonary vasculature. Low pressure baroreceptors are also referred to as volume receptors and cardiopulmonary baroreceptors.
Cardiac physiology or heart function is the study of healthy, unimpaired function of the heart: involving blood flow; myocardium structure; the electrical conduction system of the heart; the cardiac cycle and cardiac output and how these interact and depend on one another.