An adenoma is a benign tumor of epithelial tissue with glandular origin, glandular characteristics, or both. Adenomas can grow from many glandular organs, including the adrenal glands, pituitary gland, thyroid, prostate, and others. Some adenomas grow from epithelial tissue in nonglandular areas but express glandular tissue structure. Although adenomas are benign, they should be treated as pre-cancerous. Over time adenomas may transform to become malignant, at which point they are called adenocarcinomas. Most adenomas do not transform. However, even though benign, they have the potential to cause serious health complications by compressing other structures and by producing large amounts of hormones in an unregulated, non-feedback-dependent manner. Some adenomas are too small to be seen macroscopically but can still cause clinical symptoms.

A benign tumor is a mass of cells (tumor) that does not invade neighboring tissue or metastasize. Compared to malignant (cancerous) tumors, benign tumors generally have a slower growth rate. Benign tumors have relatively well differentiated cells. They are often surrounded by an outer surface or stay contained within the epithelium. Common examples of benign tumors include moles and uterine fibroids.

Pseudomyxoma peritonei (PMP) is a clinical condition caused by cancerous cells that produce abundant mucin or gelatinous ascites. The tumors cause fibrosis of tissues and impede digestion or organ function, and if left untreated, the tumors and mucin they produce will fill the abdominal cavity. This will result in compression of organs and will destroy the function of the colon, small intestine, stomach, or other organs. Prognosis with treatment in many cases is optimistic, but the disease is lethal if untreated, with death occurring via cachexia, bowel obstruction, or other types of complications.

A carcinoid is a slow-growing type of neuroendocrine tumor originating in the cells of the neuroendocrine system. In some cases, metastasis may occur. Carcinoid tumors of the midgut are associated with carcinoid syndrome.
The International Classification of Diseases for Oncology (ICD-O) is a domain-specific extension of the International Statistical Classification of Diseases and Related Health Problems for tumor diseases. This classification is widely used by cancer registries.
Carcinoid syndrome is a paraneoplastic syndrome comprising the signs and symptoms that occur secondary to neuroendocrine tumors. The syndrome is caused by neuroendocrine tumors most often found in the gut releasing biologically active substances into the blood causing symptoms such as flushing and diarrhea, and less frequently, heart failure, vomiting and bronchoconstriction.

Neuroendocrine tumors (NETs) are neoplasms that arise from cells of the endocrine (hormonal) and nervous systems. They most commonly occur in the intestine, where they are often called carcinoid tumors, but they are also found in the pancreas, lung, and the rest of the body.

Appendix cancer, also known as appendiceal cancer, is a very rare malignant tumor that forms in the vermiform appendix.

Neprilysin is an enzyme that in humans is encoded by the MME gene. Neprilysin is a zinc-dependent metalloprotease that cleaves peptides at the amino side of hydrophobic residues and inactivates several peptide hormones including glucagon, enkephalins, substance P, neurotensin, oxytocin, and bradykinin. It also degrades the amyloid beta peptide whose abnormal folding and aggregation in neural tissue has been implicated as a cause of Alzheimer's disease. Synthesized as a membrane-bound protein, the neprilysin ectodomain is released into the extracellular domain after it has been transported from the Golgi apparatus to the cell surface.

Adenocarcinoma in situ (AIS) of the lung —previously included in the category of "bronchioloalveolar carcinoma" (BAC)—is a subtype of lung adenocarcinoma. It tends to arise in the distal bronchioles or alveoli and is defined by a non-invasive growth pattern. This small solitary tumor exhibits pure alveolar distribution and lacks any invasion of the surrounding normal lung. If completely removed by surgery, the prognosis is excellent with up to 100% 5-year survival.

Mucinous cystadenoma is a benign cystic tumor lined by a mucinous epithelium. It is a type of cystic adenoma (cystadenoma).
Aggressive digital papillary adenocarcinoma, also known as digital papillary adenocarcinoma and papillary adenoma is a cutaneous condition characterized by an aggressive malignancy involving the digit between the nailbed and the distal interphalangeal joint spaces. Genetic studies reveal that human papilloma virus HPV42 is the likely driving virus in this cancer.

Metanephric adenoma (MA) is a rare, benign tumour of the kidney, that can have a microscopic appearance similar to a nephroblastoma, or a papillary renal cell carcinoma.
A sialoblastoma is a low-grade salivary gland neoplasm that recapitulates primitive salivary gland anlage. It has previously been referred to as congenital basal cell adenoma, embryoma, or basaloid adenocarcinoma. It is an extremely rare tumor, with less than 100 cases reported worldwide.
A ceruminous adenoma is a benign glandular neoplasm which arises from the ceruminous glands located within the external auditory canal. These glands are found within the outer one third to one half of the external auditory canal, more common along the posterior surface; therefore, the tumor develops within a very specific location.

An endolymphatic sac tumor (ELST) is a very uncommon papillary epithelial neoplasm arising within the endolymphatic sac or endolymphatic duct. This tumor shows a very high association with Von Hippel–Lindau syndrome (VHL).

Ceruminous adenocarcinoma is a malignant neoplasm derived from ceruminous glands of the external auditory canal. This tumor is rare, with several names used in the past. Synonyms have included cylindroma, ceruminoma, ceruminous adenocarcinoma, not otherwise specified (NOS), ceruminous adenoid cystic carcinoma (ACC), and ceruminous mucoepidermoid carcinoma.
Neuroendocrine differentiation is a term primarily used in relation to prostate cancers that display a significant neuroendocrine cell population on histopathological examination. These types of prostate cancer comprise true neuroendocrine cancers, such as small cell carcinoma, carcinoid and carcinoid-like tumors, as well as prostatic adenocarcinoma exhibiting focal neuroendocrine phenotype.
Diffuse idiopathic pulmonary neuroendocrine cell hyperplasia (DIPNECH) is a diffuse parenchymal lung disease which often presents with symptoms of cough and shortness of breath. The pathological definition published by the World Health Organization is “a generalized proliferation of scattered single cells, small nodules, or linear proliferations of pulmonary neuroendocrine (PNE) cells that may be confined to the bronchial and bronchiolar epithelium.” The true prevalence of this disease is not known. To date, just under 200 cases have been reported in the literature. However, with an increase in recognition of this disease by radiologists and pulmonologists, the number of cases has been increasing. DIPNECH predominantly affects middle-aged women with slowly progressive lung obstruction. DIPNECH is usually discovered in one of two ways: 1) as an unexpected finding following a lung surgery; or 2) by evaluation of a patient in a pulmonary clinic with longstanding, unexplained symptoms.

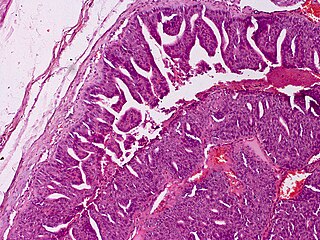
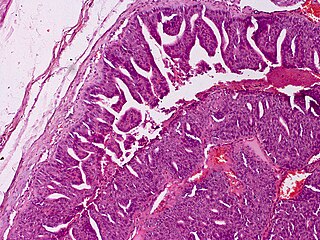
The histopathology of colorectal cancer of the adenocarcinoma type involves analysis of tissue taken from a biopsy or surgery. A pathology report contains a description of the microscopical characteristics of the tumor tissue, including both tumor cells and how the tumor invades into healthy tissues and finally if the tumor appears to be completely removed. The most common form of colon cancer is adenocarcinoma, constituting between 95% and 98% of all cases of colorectal cancer. Other, rarer types include lymphoma, adenosquamous and squamous cell carcinoma. Some subtypes have been found to be more aggressive.