Anesthesia is a state of controlled, temporary loss of sensation or awareness that is induced for medical or veterinary purposes. It may include some or all of analgesia, paralysis, amnesia, and unconsciousness. An individual under the effects of anesthetic drugs is referred to as being anesthetized.
Local anesthesia is any technique to induce the absence of sensation in a specific part of the body, generally for the aim of inducing local analgesia, that is, local insensitivity to pain, although other local senses may be affected as well. It allows patients to undergo surgical and dental procedures with reduced pain and distress. In many situations, such as cesarean section, it is safer and therefore superior to general anesthesia.

A local anesthetic (LA) is a medication that causes absence of pain sensation. In the context of surgery, a local anesthetic creates an absence of pain in a specific location of the body without a loss of consciousness, as opposed to a general anesthetic. When it is used on specific nerve pathways, paralysis also can be achieved.

General anaesthesia (UK) or general anesthesia (US) is a medically induced loss of consciousness that renders the patient unarousable even with painful stimuli. This effect is achieved by administering either intravenous or inhalational general anaesthetic medications, which often act in combination with an analgesic and neuromuscular blocking agent. Spontaneous ventilation is often inadequate during the procedure and intervention is often necessary to protect the airway. General anaesthesia is generally performed in an operating theater to allow surgical procedures that would otherwise be intolerably painful for a patient, or in an intensive care unit or emergency department to facilitate endotracheal intubation and mechanical ventilation in critically ill patients.

Anesthesiology, anaesthesiology, or anaesthesia is the medical specialty concerned with the total perioperative care of patients before, during and after surgery. It encompasses anesthesia, intensive care medicine, critical emergency medicine, and pain medicine. A physician specialized in anesthesiology is called an anesthesiologist, anaesthesiologist, or anaesthetist, depending on the country. In some countries, the terms are synonymous, while in other countries they refer to different positions, and anesthetist is only used for non-physicians, such as nurse anesthetists.

Spinal anaesthesia, also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial regional anaesthesia involving the injection of a local anaesthetic or opioid into the subarachnoid space, generally through a fine needle, usually 9 cm (3.5 in) long. It is a safe and effective form of anesthesia usually performed by anesthesiologists that can be used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus. The local anesthetic with or without an opioid injected into the cerebrospinal fluid provides locoregional anaesthesia: true analgesia, motor, sensory and autonomic (sympathic) blockade. Administering analgesics in the cerebrospinal fluid without a local anaesthetic produces locoregional analgesia: markedly reduced pain sensation, some autonomic blockade, but no sensory or motor block. Locoregional analgesia, due to mainly the absence of motor and sympathic block may be preferred over locoregional anaesthesia in some postoperative care settings. The tip of the spinal needle has a point or small bevel. Recently, pencil point needles have been made available.
Awareness under anesthesia, also referred to as intraoperative awareness or accidental awareness during general anesthesia (AAGA), is a rare complication of general anesthesia where patients regain varying levels of consciousness during their surgical procedures. While anesthesia awareness is possible without resulting in any long-term memory, it is also possible for the victim to have awareness with explicit recall, where victims can remember the events related to their surgery.

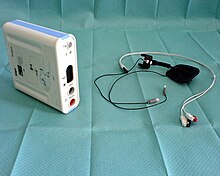
Bispectral index (BIS) is one of several technologies used to monitor depth of anesthesia. BIS monitors are used to supplement Guedel's classification system for determining depth of anesthesia. Titrating anesthetic agents to a specific bispectral index during general anesthesia in adults allows the anesthetist to adjust the amount of anesthetic agent to the needs of the patient, possibly resulting in a more rapid emergence from anesthesia. Use of the BIS monitor could reduce the incidence of intraoperative awareness during anaesthesia. The exact details of the algorithm used to create the BIS index have not been disclosed by the company that developed it.
In advanced airway management, rapid sequence induction (RSI) – also referred to as rapid sequence intubation or as rapid sequence induction and intubation (RSII) or as crash induction – is a special process for endotracheal intubation that is used where the patient is at a high risk of pulmonary aspiration. It differs from other techniques for inducing general anesthesia in that several extra precautions are taken to minimize the time between giving the induction drugs and securing the tube, during which period the patient's airway is essentially unprotected.

Tubocurarine is a toxic alkaloid historically known for its use as an arrow poison. In the mid-1900s, it was used in conjunction with an anesthetic to provide skeletal muscle relaxation during surgery or mechanical ventilation. It is now rarely used as an adjunct for clinical anesthesia because safer alternatives, such as cisatracurium and rocuronium, are available.

Neuromuscular-blocking drugs block neuromuscular transmission at the neuromuscular junction, causing paralysis of the affected skeletal muscles. This is accomplished via their action on the post-synaptic acetylcholine (Nm) receptors.

Atracurium besilate, also known as atracurium besylate, is a medication used in addition to other medications to provide skeletal muscle relaxation during surgery or mechanical ventilation. It can also be used to help with endotracheal intubation but suxamethonium (succinylcholine) is generally preferred if this needs to be done quickly. It is given by injection into a vein. Effects are greatest at about 4 minutes and last for up to an hour.

Sugammadex, sold under the brand name Bridion, is a medication for the reversal of neuromuscular blockade induced by rocuronium and vecuronium in general anaesthesia. It is the first selective relaxant binding agent (SRBA). It is marketed by Merck.
Guedel's classification is a means of assessing of depth of general anesthesia introduced by Arthur Ernest Guedel (1883-1956) in 1920.

Gantacurium chloride is a new experimental neuromuscular blocking drug or skeletal muscle relaxant in the category of non-depolarizing neuromuscular-blocking drugs, used adjunctively in surgical anesthesia to facilitate endotracheal intubation and to provide skeletal muscle relaxation during surgery or mechanical ventilation. Gantacurium is not yet available for widespread clinical use: it is currently undergoing Phase III clinical development.

Brachial plexus block is a regional anesthesia technique that is sometimes employed as an alternative or as an adjunct to general anesthesia for surgery of the upper extremity. This technique involves the injection of local anesthetic agents in close proximity to the brachial plexus, temporarily blocking the sensation and ability to move the upper extremity. The subject can remain awake during the ensuing surgical procedure, or they can be sedated or even fully anesthetized if necessary.

An acceleromyograph is a piezoelectric myograph, used to measure the force produced by a muscle after it has undergone nerve stimulation. Acceleromyographs may be used, during anaesthesia when muscle relaxants are administered, to measure the depth of neuromuscular blockade and to assess adequacy of recovery from these agents at the end of surgery. Acceleromyography is classified as quantitative neuromuscular monitoring.

Postoperative residual curarization (PORC) or residual neuromuscular blockade (RNMB) is a residual paresis after emergence from general anesthesia that may occur with the use of neuromuscular-blocking drugs. Today residual neuromuscular blockade is defined as a train of four ratio of less than 0.9 when measuring the response to ulnar nerve stimulation at the adductor pollicis muscle using mechanomyography or electromyography. A meta-analysis reported that the incidence of residual neuromuscular paralysis was 41% in patients receiving intermediate neuromuscular blocking agents during anaesthesia. It is possible that > 100,000 patients annually in the USA alone, are at risk of adverse events associated with undetected residual neuromuscular blockade. Neuromuscular function monitoring and the use of the appropriate dosage of sugammadex to reverse blockade produced by rocuronium can reduce the incidence of postoperative residual curarization. In this study, with usual care group receiving reversal with neostigmine resulted in a residual blockade rate of 43%.
The following outline is provided as an overview of and topical guide to anesthesia:
Neuromuscular blocking agents, or in abbreviation, NMBAs, are chemical agents that paralyse skeletal muscles by blocking the movement of neurotransmitter at the neuromuscular junction. They are often used during general anesthesia to optimize intubating and surgical conditions, specifically to facilitate endotracheal intubation. This class of medications helps to reduce patient movement, breathing, or ventilator dyssynchrony and allows lower insufflation pressures during laparoscopy including the generation of nerve impulses. It has several indications for use in the intense care unit. It can help reduce hoarseness in voice as well as injury to the vocal cord during intubation. In addition, it plays an important role in facilitating mechanical ventilation in patients with poor lung function. In the following section, neuromuscular blocking agent's history, usages, mechanisms, side effects, interactions and pharmacology will further be elaborated and discussed.