An anesthetic or anaesthetic is a drug used to induce anesthesia — in other words, to result in a temporary loss of sensation or awareness. They may be divided into two broad classes: general anesthetics, which result in a reversible loss of consciousness, and local anesthetics, which cause a reversible loss of sensation for a limited region of the body without necessarily affecting consciousness.
Awareness under anesthesia, also referred to as intraoperative awareness or accidental awareness during general anesthesia (AAGA), is a rare complication of general anesthesia where patients regain varying levels of consciousness during their surgical procedures. While anesthesia awareness is possible without resulting in any long-term memory, it is also possible for the victim to have awareness with explicit recall, where victims can remember the events related to their surgery.

A neuromuscular junction is a chemical synapse between a motor neuron and a muscle fiber.

Dantrolene sodium, sold under the brand name Dantrium among others, is a postsynaptic muscle relaxant that lessens excitation-contraction coupling in muscle cells. It achieves this by inhibiting Ca2+ ions release from sarcoplasmic reticulum stores by antagonizing ryanodine receptors. It is the primary drug used for the treatment and prevention of malignant hyperthermia, a rare, life-threatening disorder triggered by general anesthesia or drugs. It is also used in the management of neuroleptic malignant syndrome, muscle spasticity (e.g. after strokes, in paraplegia, cerebral palsy, or patients with multiple sclerosis), and poisoning by 2,4-dinitrophenol or by the related compounds dinoseb and dinoterb.

Bispectral index (BIS) is one of several technologies used to monitor depth of anesthesia. BIS monitors are used to supplement Guedel's classification system for determining depth of anesthesia. Titrating anesthetic agents to a specific bispectral index during general anesthesia in adults allows the anesthetist to adjust the amount of anesthetic agent to the needs of the patient, possibly resulting in a more rapid emergence from anesthesia. Use of the BIS monitor could reduce the incidence of intraoperative awareness during anaesthesia. The exact details of the algorithm used to create the BIS index have not been disclosed by the company that developed it.

Tubocurarine is a toxic alkaloid historically known for its use as an arrow poison. In the mid-1900s, it was used in conjunction with an anesthetic to provide skeletal muscle relaxation during surgery or mechanical ventilation. It is now rarely used as an adjunct for clinical anesthesia because safer alternatives, such as cisatracurium and rocuronium, are available.

Neuromuscular-blocking drugs block neuromuscular transmission at the neuromuscular junction, causing paralysis of the affected skeletal muscles. This is accomplished via their action on the post-synaptic acetylcholine (Nm) receptors.
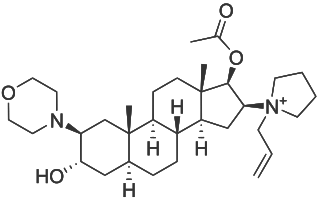
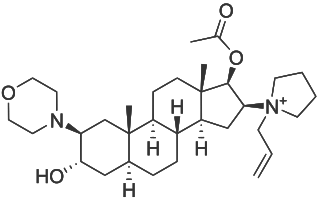
Rocuronium bromide is an aminosteroid non-depolarizing neuromuscular blocker or muscle relaxant used in modern anaesthesia to facilitate tracheal intubation by providing skeletal muscle relaxation, most commonly required for surgery or mechanical ventilation. It is used for standard endotracheal intubation, as well as for rapid sequence induction (RSI).

A piezoelectric sensor is a device that uses the piezoelectric effect to measure changes in pressure, acceleration, temperature, strain, or force by converting them to an electrical charge. The prefix piezo- is Greek for 'press' or 'squeeze'.

Fenoldopam mesylate (Corlopam) is a drug and synthetic benzazepine derivative which acts as a selective D1 receptor partial agonist. Fenoldopam is used as an antihypertensive agent. It was approved by the Food and Drug Administration (FDA) in September 1997.

Capreomycin is an antibiotic which is given in combination with other antibiotics for the treatment of tuberculosis. Specifically it is a second line treatment used for active drug resistant tuberculosis. It is given by injection into a vein or muscle.

Sugammadex, sold under the brand name Bridion, is a medication for the reversal of neuromuscular blockade induced by rocuronium and vecuronium in general anaesthesia. It is the first selective relaxant binding agent (SRBA). It is marketed by Merck.
Guedel's classification is a means of assessing of depth of general anesthesia introduced by Arthur Ernest Guedel (1883-1956) in 1920.

A piezoelectric accelerometer is an accelerometer that employs the piezoelectric effect of certain materials to measure dynamic changes in mechanical variables.

Gantacurium chloride is a new experimental neuromuscular blocking drug or skeletal muscle relaxant in the category of non-depolarizing neuromuscular-blocking drugs, used adjunctively in surgical anesthesia to facilitate endotracheal intubation and to provide skeletal muscle relaxation during surgery or mechanical ventilation. Gantacurium is not yet available for widespread clinical use: it is currently undergoing Phase III clinical development.
Postanesthetic shivering (PAS) is shivering after anesthesia.

In anesthesia, neuromuscular blocking agents may be required to facilitate endotracheal intubation and provide optimal surgical conditions. When neuromuscular blocking agents are administered, neuromuscular function of the patient must be monitored. Neuromuscular function monitoring is a technique that involves the electrical stimulation of a motor nerve and monitoring the response of the muscle supplied by that nerve. It may be used from the induction of to recovery from neuromuscular blockade. Importantly, it is used to confirm adequacy of recovery after the administration of neuromuscular blocking agents. The response of the muscles to electrical stimulation of the nerves can be recorded subjectively (qualitative) or objectively (quantitatively). Quantitative techniques include electromyography, acceleromyography, kinemyography, phonomygraphy and mechanomyography. Neuromuscular monitoring is recommended when neuromuscular-blocking drugs have been part of the general anesthesia and the doctor wishes to avoid postoperative residual curarization (PORC) in the patient, that is, the residual paralysis of muscles stemming from these drugs.

Postoperative residual curarization (PORC) or residual neuromuscular blockade (RNMB) is a residual paresis after emergence from general anesthesia that may occur with the use of neuromuscular-blocking drugs. Today residual neuromuscular blockade is defined as a train of four ratio of less than 0.9 when measuring the response to ulnar nerve stimulation at the adductor pollicis muscle using mechanomyography or electromyography. A meta-analysis reported that the incidence of residual neuromuscular paralysis was 41% in patients receiving intermediate neuromuscular blocking agents during anaesthesia. It is possible that > 100,000 patients annually in the USA alone, are at risk of adverse events associated with undetected residual neuromuscular blockade. Neuromuscular function monitoring and the use of the appropriate dosage of sugammadex to reverse blockade produced by rocuronium can reduce the incidence of postoperative residual curarization. In this study, with usual care group receiving reversal with neostigmine resulted in a residual blockade rate of 43%.
A respiratory pressure meter measures the maximum inspiratory and expiratory pressures that a patient can generate at either the mouth (MIP and MEP) or inspiratory pressure a patient can generate through their nose via a sniff manoeuvre (SNIP). These measurements require patient cooperation and are known as volitional tests of respiratory muscle strength. Handheld devices displaying the measurement achieved in cmH2O and the pressure trace created, allow quick patient testing away from the traditional pulmonary laboratory and are useful for ward based, out patient, and preoperative assessment as well as for use by pulmonologists and physiotherapists.
Neuromuscular blocking agents, or in abbreviation, NMBAs, are chemical agents that paralyse skeletal muscles by blocking the movement of neurotransmitter at the neuromuscular junction. They are often used during general anesthesia to optimize intubating and surgical conditions, specifically to facilitate endotracheal intubation. This class of medications helps to reduce patient movement, breathing, or ventilator dyssynchrony and allows lower insufflation pressures during laparoscopy including the generation of nerve impulses. It has several indications for use in the intense care unit. It can help reduce hoarseness in voice as well as injury to the vocal cord during intubation. In addition, it plays an important role in facilitating mechanical ventilation in patients with poor lung function. In the following section, neuromuscular blocking agent's history, usages, mechanisms, side effects, interactions and pharmacology will further be elaborated and discussed.