Related Research Articles

The blood–brain barrier (BBB) is a highly selective semipermeable border of endothelial cells that regulates the transfer of solutes and chemicals between the circulatory system and the central nervous system, thus protecting the brain from harmful or unwanted substances in the blood. The blood–brain barrier is formed by endothelial cells of the capillary wall, astrocyte end-feet ensheathing the capillary, and pericytes embedded in the capillary basement membrane. This system allows the passage of some small molecules by passive diffusion, as well as the selective and active transport of various nutrients, ions, organic anions, and macromolecules such as glucose and amino acids that are crucial to neural function.

The lipid bilayer is a thin polar membrane made of two layers of lipid molecules. These membranes are flat sheets that form a continuous barrier around all cells. The cell membranes of almost all organisms and many viruses are made of a lipid bilayer, as are the nuclear membrane surrounding the cell nucleus, and membranes of the membrane-bound organelles in the cell. The lipid bilayer is the barrier that keeps ions, proteins and other molecules where they are needed and prevents them from diffusing into areas where they should not be. Lipid bilayers are ideally suited to this role, even though they are only a few nanometers in width, because they are impermeable to most water-soluble (hydrophilic) molecules. Bilayers are particularly impermeable to ions, which allows cells to regulate salt concentrations and pH by transporting ions across their membranes using proteins called ion pumps.

A liposome is a small artificial vesicle, spherical in shape, having at least one lipid bilayer. Due to their hydrophobicity and/or hydrophilicity, biocompatibility, particle size and many other properties, liposomes can be used as drug delivery vehicles for administration of pharmaceutical drugs and nutrients, such as lipid nanoparticles in mRNA vaccines, and DNA vaccines. Liposomes can be prepared by disrupting biological membranes.

ADME is the four-letter abbreviation (acronym) for absorption, distribution, metabolism, and excretion, and is mainly used in fields such as pharmacokinetics and pharmacology. The four letter stands for descriptors quantifying how a given drug interacts within body over time. The term ADME was first introduced in the 1960s, and has become a standard term widely used in scientific literature, teaching, drug regulations, and clinical practice.

The MTT assay is a colorimetric assay for assessing cell metabolic activity. NAD(P)H-dependent cellular oxidoreductase enzymes may, under defined conditions, reflect the number of viable cells present. These enzymes are capable of reducing the tetrazolium dye MTT, which is chemically 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide, to its insoluble formazan, which has a purple color. Other closely related tetrazolium dyes including XTT, MTS and the WSTs, are used in conjunction with the intermediate electron acceptor, 1-methoxy phenazine methosulfate (PMS). With WST-1, which is cell-impermeable, reduction occurs outside the cell via plasma membrane electron transport. However, this traditionally assumed explanation is currently contended as proof has also been found of MTT reduction to formazan in lipidic cellular structures without apparent involvement of oxidoreductases.

Caco-2 is an immortalized cell line of human colorectal adenocarcinoma cells. It is primarily used as a model of the intestinal epithelial barrier. In culture, Caco-2 cells spontaneously differentiate into a heterogeneous mixture of intestinal epithelial cells. It was developed in 1977 by Jorgen Fogh at the Sloan-Kettering Institute for Cancer Research.
The Biopharmaceutics Classification System (BCS) is a system to differentiate drugs on the basis of their solubility and permeability.
Absorption is the journey of a drug travelling from the site of administration to the site of action.
Skin absorption is a route by which substances can enter the body through the skin. Along with inhalation, ingestion and injection, dermal absorption is a route of exposure for toxic substances and route of administration for medication. Absorption of substances through the skin depends on a number of factors, the most important of which are concentration, duration of contact, solubility of medication, and physical condition of the skin and part of the body exposed.

Transdermal is a route of administration wherein active ingredients are delivered across the skin for systemic distribution. Examples include transdermal patches used for medicine delivery. The drug is administered in the form of a patch or ointment that delivers the drug into the circulation for systemic effect.
A self-microemulsifying drug delivery system (SMEDDS) is a drug delivery system that uses a microemulsion achieved by chemical rather than mechanical means. That is, by an intrinsic property of the drug formulation, rather than by special mixing and handling. It employs the familiar ouzo effect displayed by anethole in many anise-flavored liquors. Microemulsions have significant potential for use in drug delivery, and SMEDDS are the best of these systems identified to date. SMEDDS are of particular value in increasing the absorption of lipophilic drugs taken by mouth.

Lipid nanoparticles (LNPs) are nanoparticles composed of lipids. They are a novel pharmaceutical drug delivery system, and a novel pharmaceutical formulation. LNPs as a drug delivery vehicle were first approved in 2018 for the siRNA drug Onpattro. LNPs became more widely known in late 2020, as some COVID-19 vaccines that use RNA vaccine technology coat the fragile mRNA strands with PEGylated lipid nanoparticles as their delivery vehicle.
Transepithelial potential difference (TEPD) is the voltage across an epithelium, and is the sum of the membrane potentials for the outer and inner cell membranes.
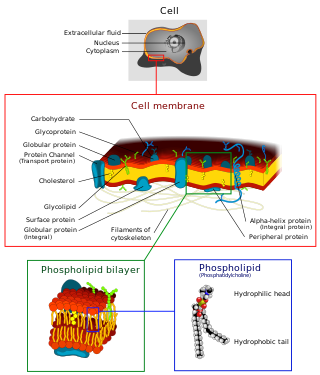
The cell membrane is a biological membrane that separates and protects the interior of a cell from the outside environment. The cell membrane consists of a lipid bilayer, made up of two layers of phospholipids with cholesterols interspersed between them, maintaining appropriate membrane fluidity at various temperatures. The membrane also contains membrane proteins, including integral proteins that span the membrane and serve as membrane transporters, and peripheral proteins that loosely attach to the outer (peripheral) side of the cell membrane, acting as enzymes to facilitate interaction with the cell's environment. Glycolipids embedded in the outer lipid layer serve a similar purpose. The cell membrane controls the movement of substances in and out of a cell, being selectively permeable to ions and organic molecules. In addition, cell membranes are involved in a variety of cellular processes such as cell adhesion, ion conductivity, and cell signalling and serve as the attachment surface for several extracellular structures, including the cell wall and the carbohydrate layer called the glycocalyx, as well as the intracellular network of protein fibers called the cytoskeleton. In the field of synthetic biology, cell membranes can be artificially reassembled.
An organ-on-a-chip (OOC) is a multi-channel 3-D microfluidic cell culture, integrated circuit (chip) that simulates the activities, mechanics and physiological response of an entire organ or an organ system. It constitutes the subject matter of significant biomedical engineering research, more precisely in bio-MEMS. The convergence of labs-on-chips (LOCs) and cell biology has permitted the study of human physiology in an organ-specific context. By acting as a more sophisticated in vitro approximation of complex tissues than standard cell culture, they provide the potential as an alternative to animal models for drug development and toxin testing.
Buccal administration is a topical route of administration by which drugs held or applied in the buccal area diffuse through the oral mucosa and enter directly into the bloodstream. Buccal administration may provide better bioavailability of some drugs and a more rapid onset of action compared to oral administration because the medication does not pass through the digestive system and thereby avoids first pass metabolism. Drug forms for buccal administration include tablets and thin films.
TNO (gastro-) Intestinal Models (“TIM”) are model systems mimicking the digestive tract. The models are dynamic computer controlled multi-compartmental systems with adjustable parameters for the physiological conditions of the stomach and intestine. Temperature, peristalsis, bile secretion, secretion of saliva, stomach and pancreas enzymes are all fully adjustable. The TIM systems are being used to study the behavior of oral products during transit through the stomach, the small intestine and large intestine. Commonly performed studies concern the digestibility of food and food components, the bioaccessibility for absorption of pharmaceutical compounds, proteins, fat, minerals and vitamins.

Ethosomes are phospholipid nanovesicles used for dermal and transdermal delivery of molecules. Ethosomes were developed by Touitou et al.,1997, as additional novel lipid carriers composed of ethanol, phospholipids, and water. They are reported to improve the skin delivery of various drugs. Ethanol is an efficient permeation enhancer that is believed to act by affecting the intercellular region of the stratum corneum. Ethosomes are soft malleable vesicles composed mainly of phospholipids, ethanol, and water. These soft vesicles represent novel vesicles carriers for enhanced delivery through the skin. The size of the ethosomes vesicles can be modulated from tens of nanometers to microns.
Topical drug delivery (TDD) is a route of drug administration that allows the topical formulation to be delivered across the skin upon application, hence producing a localized effect to treat skin disorders like eczema. The formulation of topical drugs can be classified into corticosteroids, antibiotics, antiseptics, and anti-fungal. The mechanism of topical delivery includes the diffusion and metabolism of drugs in the skin. Historically, topical route was the first route of medication used to deliver drugs in humans in ancient Egyptian and Babylonian in 3000 BCE. In these ancient cities, topical medications like ointments and potions were used on the skin. The delivery of topical drugs needs to pass through multiple skin layers and undergo pharmacokinetics, hence factor like dermal diseases minimize the bioavailability of the topical drugs. The wide use of topical drugs leads to the advancement in topical drug delivery. These advancements are used to enhance the delivery of topical medications to the skin by using chemical and physical agents. For chemical agents, carriers like liposomes and nanotechnologies are used to enhance the absorption of topical drugs. On the other hand, physical agents, like micro-needles is other approach for enhancement ofabsorption. Besides using carriers, other factors such as pH, lipophilicity, and drug molecule size govern the effectiveness of topical formulation.
In medicinal chemistry, Drug Permeability is an empirical parameter that indicates the likelihood of a chemical entity or an active pharmaceutical ingredient to cross biological barrier and to became bioavailable in the body. Drug permeability, together with drug aqueous solubility are the two parameters which defines the fate of the active ingredient after oral administration that ultimately defines its bioavailability. When drug permeability is empirically measured in vitro, it is generally called apparent permeability (Papp) as its absolute value varies according to the method selected for its measurement. Papp is measured in vitro utilizing cellular based barriers such as the Caco-2 model or utilizing artificial biomimetic barriers, such as the Parallel Artificial Membrane Permeation Assay (PAMPA) or the PermeaPad. All these methods are built on an acceptor compartment where the drug solution is placed, a biomimetic barrier and an acceptor compartment, where the drug concentration is quantified over time. By maintaining sink condition, a steady state is reached after a lag time.
References
- ↑ Ottaviani, Giorgio; Martel, Sophie; Carrupt, Pierre-Alain (2006). "Parallel Artificial Membrane Permeability Assay: A New Membrane for the Fast Prediction of Passive Human Skin Permeability". Journal of Medicinal Chemistry. 49 (13): 3948–3954. doi:10.1021/jm060230+. ISSN 0022-2623. PMID 16789751.
- ↑ Bermejo, M. et al. (2004). PAMPA – a drug absorption in vitro model 7. Comparing rat in situ, Caco-2, and PAMPA permeability of fluoroquinolones. Pharm. Sci., 21: 429-441.
- ↑ Avdeef, A. et al. (2005). Caco-2 permeability of weakly basic drugs predicted with the Double-Sink PAMPA pKaflux method. Pharm. Sci., 24: 333-349.
- ↑ Avdeef, A. et al. (2004). PAMPA – a drug absorption in vitro model 11. Matching the in vivo unstirred water layer thickness by individual-well stirring in microtitre plates. Pharm. Sci., 22: 365-374.
- ↑ Dagenais, C. et al. (2009). P-glycoprotein deficient mouse in situ blood–brain barrier permeability and its prediction using an in combo PAMPA model. Eur. J. Phar. Sci., 38(2): 121-137.
- ↑ Artursson, P. Application of physicochemical properties of molecules to predict intestinal permeability. AAPS Workshop on Permeability Definitions and Regulatory Standards, Arlington, VA, USA (1998) 17-19 Aug.
- ↑ Kansy M, Senner F, Gubernator K. (1998) Physicochemical high throughput screening: parallel artificial membrane permeability assay in the description of passive absorption processes. J. Med. Chem. 41: 1007–1010.
- ↑ Chen, X. et al. (2008) A Novel Design of Artificial Membrane for Improving the PAMPA Model. Pharmaceutical Research, 25: 1511.