Urology, also known as genitourinary surgery, is the branch of medicine that focuses on surgical and medical diseases of the male and female urinary-tract system and the male reproductive organs. Organs under the domain of urology include the kidneys, adrenal glands, ureters, urinary bladder, urethra, and the male reproductive organs.

Prune belly syndrome is a rare, genetic birth defect affecting about 1 in 40,000 births. About 97% of those affected are male. Prune belly syndrome is a congenital disorder of the urinary system, characterized by a triad of symptoms. The syndrome is named for the mass of wrinkled skin that is often present on the abdomen of those with the disorder.
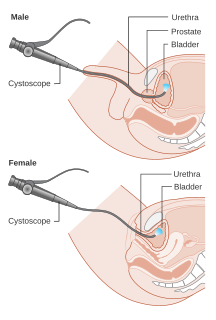
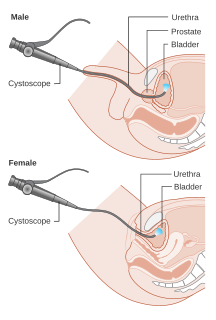
Cystoscopy is endoscopy of the urinary bladder via the urethra. It is carried out with a cystoscope.

Hypospadias is a common variation in fetal development of the penis in which the urethra does not open from its usual location in the head of the penis. It is the second-most common birth abnormality of the male reproductive system, affecting about one of every 250 males at birth. Roughly 90% of cases are the less serious distal hypospadias, in which the urethral opening is on or near the head of the penis (glans). The remainder have proximal hypospadias, in which the meatus is all the way back on the shaft of the penis, near or within the scrotum. Shiny tissue that should have made the urethra extends from the meatus to the tip of the glans; this tissue is called the urethral plate.

An epispadias is a rare type of malformation in which the urethra ends, in males, in an opening on the upper aspect of the penis, and in females when the urethra develops too far anteriorly. It occurs in around 1 in 120,000 male and 1 in 500,000 female births.

Hematuria or haematuria is defined as the occurrence of blood or red blood cells in the urine. The word hematuria is derived from Greek haima (αἷμα) "blood" and ouron (οὖρον) "urine". Hematuria can be visible to the naked eye and may appear red or brown, or it can be microscopic. The origin of the blood that enters and mixes with the urine can arise from any anatomical site within the urinary system, including the kidney, ureter, urinary bladder, and urethra, and in men, the prostate. Common causes of hematuria include urinary tract infection (UTI), kidney stones, viral illness, trauma, bladder cancer, and exercise. The underlying causes of hematuria can be divided into glomerular and non-glomerular causes, referring to the involvement of the glomerulus of the kidney. Notably, not all red urine is hematuria. Other substances such as certain medications and foods can cause urine to appear red. Menstruation in women may also cause the appearance of hematuria and may result in a positive urine dipstick test for hematuria. Additionally, a urine dipstick test may be falsely positive for hematuria due to other substances in the urine such as myoglobin during rhabdomyolysis. A positive urine dipstick test should be confirmed with microscopy, where hematuria is defined by three of more red blood cells per high power field. When hematuria is detected, a thorough history and physical examination with appropriate further evaluation can help determine the underlying cause.

The genitourinary system, or urogenital system, are the organs of the reproductive system and the urinary system. These are grouped together because of their proximity to each other, their common embryological origin and the use of common pathways, like the male urethra. Also, because of their proximity, the systems are sometimes imaged together.

Pediatric surgery is a subspecialty of surgery involving the surgery of fetuses, infants, children, adolescents, and young adults.

Bladder exstrophy is a congenital anomaly that exists along the spectrum of the exstrophy-epispadias complex, and most notably involves protrusion of the urinary bladder through a defect in the abdominal wall. Its presentation is variable, often including abnormalities of the bony pelvis, pelvic floor, and genitalia. The underlying embryologic mechanism leading to bladder exstrophy is unknown, though it is thought to be in part due to failed reinforcement of the cloacal membrane by underlying mesoderm. Exstrophy means the inversion of a hollow organ.
Hydronephrosis describes hydrostatic dilation of the renal pelvis and calyces as a result of obstruction to urine flow downstream. Alternatively, hydroureter describes the dilation of the ureter, and hydronephroureter describes the dilation of the entire upper urinary tract.

An imperforate anus or anorectal malformations (ARMs) are birth defects in which the rectum is malformed. ARMs are a spectrum of different congenital anomalies which vary from fairly minor lesions to complex anomalies. The cause of ARMs is unknown; the genetic basis of these anomalies is very complex because of their anatomical variability. In 8% of patients, genetic factors are clearly associated with ARMs. Anorectal malformation in Currarino syndrome represents the only association for which the gene HLXB9 has been identified.

The Mitrofanoff procedure also known as the Mitrofanoff appendicovesicostomy, is a surgical procedure in which the appendix is used to create a conduit, or channel, between the skin surface and the urinary bladder. The small opening on the skin surface, or the stoma, is typically located either in the navel or nearby the navel on the right lower side of the abdomen. Originally developed by Professor Paul Mitrofanoff in 1980, the procedure represents an alternative to urethral catheterization and is sometimes used by people with urethral damage or by those with severe autonomic dysreflexia. An intermittent catheter, or a catheter that is inserted and then removed after use, is typically passed through the channel every 3–4 hours and the urine is drained into a toilet or a bottle. As the bladder fills, rising pressure compresses the channel against the bladder wall, creating a one-way valve that prevents leakage of urine between catheterizations.

Posterior urethral valve (PUV) disorder is an obstructive developmental anomaly in the urethra and genitourinary system of male newborns. A posterior urethral valve is an obstructing membrane in the posterior male urethra as a result of abnormal in utero development. It is the most common cause of bladder outlet obstruction in male newborns. The disorder varies in degree, with mild cases presenting late due to milder symptoms. More severe cases can have renal and respiratory failure from lung underdevelopment as result of low amniotic fluid volumes, requiring intensive care and close monitoring. It occurs in about one in 8,000 babies.
In urology, voiding cystourethrography (VCUG) is a frequently performed technique for visualizing a person's urethra and urinary bladder while the person urinates (voids). It is used in the diagnosis of vesicoureteral reflux, among other disorders. The technique consists of catheterizing the person in order to fill the bladder with a radiocontrast agent, typically diatrizoic acid. Under fluoroscopy the radiologist watches the contrast enter the bladder and looks at the anatomy of the patient. If the contrast moves into the ureters and back into the kidneys, the radiologist makes the diagnosis of vesicoureteral reflux, and gives the degree of severity a score. The exam ends when the person voids while the radiologist is watching under fluoroscopy. Consumption of fluid promotes excretion of contrast media after the procedure. It is important to watch the contrast during voiding, because this is when the bladder has the most pressure, and it is most likely this is when reflux will occur. Despite this detailed description of the procedure, at least as of 2016 the technique had not been standardized across practices.
Urogynecology or urogynaecology is a surgical sub-specialty of urology and gynecology.

Diphallia, penile duplication (PD), diphallic terata, or diphallasparatus, is an extremely rare developmental abnormality in which a male is born with two penises. The first reported case was by Johannes Jacob Wecker in 1609. Its occurrence is 1 in 5.5 million boys in the United States.
Bladder outlet obstruction occurs when urine is unable to flow from the kidneys through the ureters and out of the bladder through the urethra. Decreased flow of urine leads to swelling of the urinary tract, called hydronephrosis. This process of decreased flow of urine through the urinary tract can begin as early as during intrauterine life and it prevents normal development of fetal kidneys and fetal urine. Low levels of fetal urine leads to low amniotic fluid levels and incomplete lung maturation. Older children and adults can also experience bladder outlet obstruction; however, this process is usually reversible and isn't associated with as many poor outcomes as in infants with congenital bladder outlet obstruction.

Aseem Ravindra Shukla is the Director of Minimally Invasive Surgery in the Department of Urology at the Children's Hospital of Philadelphia, PA and is a Professor of Surgery (Urology) at the Perelman School of Medicine at the University of Pennsylvania. Shukla is the co-founder and board member of the Hindu American Foundation.

Vaginal anomalies are abnormal structures that are formed during the prenatal development of the female reproductive system and are rare congenital defects that result in an abnormal or absent vagina. When present, they are often found with uterine, skeletal and urinary abnormalities. This is because these structures, like the vagina, are most susceptible to disruption during crucial times of organ-genesis. Many of these defects are classified under the broader term Müllerian duct anomalies. Müllerian duct anomalies are caused by a disturbance during the embryonic time of genitourinary development. The other isolated incidents of vaginal anomalies can occur with no apparent cause. Oftentimes vaginal anomalies are part of a cluster of defects or syndromes. In addition, inheritance can play a part as can prenatal exposure to some teratogens. Many vaginal anomalies are not detected at birth because the external genitalia appear to be normal. Other organs of the reproductive system may not be affected by an abnormality of the vagina. The uterus, fallopian tubes and ovaries can be functional despite the presence of a defect of the vagina and external genitalia. A vaginal anomaly may not affect fertility. Though it depends on the extent of the vaginal defect, it is possible for conception to occur. In instances where a functional ovary exists, IVF may be successful. Functioning ovaries in a woman with a vaginal defect allows the implantation of a fertilized ovum into the uterus of an unaffected gestational carrier, usually another human. A successful conception and can occur. Vaginal length varies from 6.5 to 12.5 cm. Since this is slightly shorter than older descriptions, it may impact the diagnosis of women with vaginal agenesis or hypoplasia who may unnecessarily be encouraged to undergo treatment to increase the size of the vagina. Vaginal anomalies may cause difficulties in urination, conception, pregnancy, impair sex. Psychosocial effects can also exist.
Kurt McCammon is a Professor and the Devine Chair in Genitourinary Reconstructive Surgery at Eastern Virginia Medical School, where he has served as the Chairman for the Department of Urology since 2011, Program Director of the Department of Urology since 2006, and Fellowship Director for the Adult and Pediatric Genitourinary Reconstructive Surgery since 2010. Additionally, he is the past president of the Society of Genitourinary Reconstructive Surgeons, on the board of the International Volunteers in Urology, and a current member of the American Urological Association Board of Directors. As a reconstructive urologist, McCammon surgically addresses urethral stricture disease, male urinary incontinence, erectile dysfunction, female urinary incontinence, genital abnormalities, and other genitourinary issues.