Related Research Articles
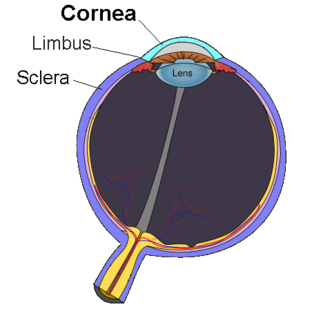
The cornea is the transparent front part of the eye that covers the iris, pupil, and anterior chamber. Along with the anterior chamber and lens, the cornea refracts light, accounting for approximately two-thirds of the eye's total optical power. In humans, the refractive power of the cornea is approximately 43 dioptres. The cornea can be reshaped by surgical procedures such as LASIK.

A route of administration in pharmacology and toxicology is the way by which a drug, fluid, poison, or other substance is taken into the body.

Benzalkonium chloride, also known as alkyldimethylbenzylammonium chloride (ADBAC) and by the trade name Zephiran, is a type of cationic surfactant. It is an organic salt classified as a quaternary ammonium compound. ADBACs have three main categories of use: as a biocide, a cationic surfactant, and a phase transfer agent. ADBACs are a mixture of alkylbenzyldimethylammonium chlorides, in which the alkyl group has various even-numbered alkyl chain lengths.

A transdermal patch is a medicated adhesive patch that is placed on the skin to deliver a specific dose of medication through the skin and into the bloodstream. An advantage of a transdermal drug delivery route over other types of medication delivery is that the patch provides a controlled release of the medication into the patient, usually through either a porous membrane covering a reservoir of medication or through body heat melting thin layers of medication embedded in the adhesive. The main disadvantage to transdermal delivery systems stems from the fact that the skin is a very effective barrier; as a result, only medications whose molecules are small enough to penetrate the skin can be delivered by this method. The first commercially available prescription patch was approved by the U.S. Food and Drug Administration in December 1979. These patches administered scopolamine for motion sickness.

A topical medication is a medication that is applied to a particular place on or in the body. Most often topical administration means application to body surfaces such as the skin or mucous membranes to treat ailments via a large range of classes including creams, foams, gels, lotions, and ointments. Many topical medications are epicutaneous, meaning that they are applied directly to the skin. Topical medications may also be inhalational, such as asthma medications, or applied to the surface of tissues other than the skin, such as eye drops applied to the conjunctiva, or ear drops placed in the ear, or medications applied to the surface of a tooth. The word topical derives from Greek τοπικόςtopikos, "of a place".

Nerolidol, also known as peruviol and penetrol, is a naturally occurring sesquiterpene alcohol found in the essential oils of many types of plants and flowers. There are two isomers of nerolidol, cis and trans, which differ in the geometry about the central double bond. Nerolidol is present in neroli, ginger, jasmine, lavender, tea tree, Cannabis sativa, and lemon grass, and is a dominant scent compound in Brassavola nodosa. The aroma of nerolidol is woody and reminiscent of fresh bark. It is used as a flavoring agent and in perfumery and is used in non-cosmetic products such as detergents and cleansers. It is currently under testing as a skin penetration enhancer for the transdermal delivery of therapeutic drugs. Additionally, it is known for various biological activities include antioxidant, anti fungal, anticancer, and antimicrobial activity. It is one of several organic volatiles produced by the Arabidopsis lyrata ssp. petraea flower in response to insect feeding. Because of its hydrophobic nature, nerolidol is easily permeable across the plasma membrane and can interact with intracellular proteins. However it has a high cytotoxic potential and can disrupt the membrane.

1-Decanol is a straight chain fatty alcohol with ten carbon atoms and the molecular formula C10H21OH. It is a colorless to light yellow viscous liquid that is insoluble in water and has an aromatic odor. The interfacial tension against water at 20 °C is 8.97 mN/m.
Sonophoresis is a method that utilizes ultrasound to enhance the delivery of topical medications through the stratum corneum, to the epidermis and dermis. Sonophoresis allows for the enhancement of the permeability of the skin along with other modalities, such as iontophoresis, to deliver drugs with lesser side effects. Currently, sonophoresis is used widely in transdermal drug delivery, but has potential applications in other sectors of drug delivery, such as the delivery of drugs to the eye and brain.
Skin absorption is a route by which substances can enter the body through the skin. Along with inhalation, ingestion and injection, dermal absorption is a route of exposure for toxic substances and route of administration for medication. Absorption of substances through the skin depends on a number of factors, the most important of which are concentration, duration of contact, solubility of medication, and physical condition of the skin and part of the body exposed.

Transdermal is a route of administration wherein active ingredients are delivered across the skin for systemic distribution. Examples include transdermal patches used for medicine delivery. The drug is administered in the form of a patch or ointment that delivers the drug into the circulation for systemic effect.
Thiolated polymers or designated thiomers are experimental polymers used in biotechnology product development with the intention to prolong mucosal drug residence time and to enhance absorption of drugs. Thiomers have thiol bearing side chains. Sulfhydryl ligands of low molecular mass are covalently bound to a polymeric backbone consisting of mainly biodegradable polymers, such as chitosan, hyaluronic acid, cellulose derivatives, pullulan, starch, gelatin, polyacrylates, cyclodextrins, or silicones.
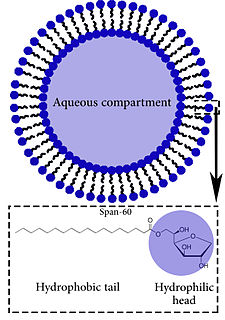
A niosome is a non-ionic surfactant-based vesicle. Niosomes are formed mostly by non-ionic surfactant and cholesterol incorporation as an excipient. They are structurally similar to liposomes as they both have a bilayer. However, the materials used to prepare niosomes are what make them more stable. They can entrap both hydrophilic and lipophilic drugs, either in an aqueous layer or in a vesicular membrane made of lipid material.
Mucoadhesion describes the attractive forces between a biological material and mucus or mucous membrane. Mucous membranes adhere to epithelial surfaces such as the gastrointestinal tract (GI-tract), the vagina, the lung, the eye, etc. They are generally hydrophilic as they contain many hydrogen macromolecules due to the large amount of water within its composition. However, mucin also contains glycoproteins that enable the formation of a gel-like substance. Understanding the hydrophilic bonding and adhesion mechanisms of mucus to biological material is of utmost importance in order to produce the most efficient applications. For example, in drug delivery systems, the mucus layer must be penetrated in order to effectively transport micro- or nanosized drug particles into the body. Bioadhesion is the mechanism by which two biological materials are held together by interfacial forces.

Cetalkonium chloride (CKC) is a quaternary ammonium compound of the alkyl-benzyldimethylammonium chloride family, the alkyl group having a chain length of C16. It is used in pharmaceutical products either as an excipient or as an active ingredient. It may be found in very small amount in the excipient benzalkonium chloride mixture. Cetalkonium chloride is purchased as a raw material in dry form as a white powder.
A nanocapsule is a nanoscale shell made from a nontoxic polymer. They are vesicular systems made of a polymeric membrane which encapsulates an inner liquid core at the nanoscale. Nanocapsules have many uses, including promising medical applications for drug delivery, food enhancement, nutraceuticals, and for self-healing materials. The benefits of encapsulation methods are for protection of these substances to protect in the adverse environment, for controlled release, and for precision targeting. Nanocapsules can potentially be used as MRI-guided nanorobots or nanobots, although challenges remain.

Joseph Kost is an Israeli academic, currently holder of The Abraham and Bessie Zacks Chair in Biomedical Engineering and the past Dean of the Faculty of Engineering Sciences at the Ben-Gurion University of the Negev.

Ethosomes are phospholipid nanovesicles used for dermal and transdermal delivery of molecules. Ethosomes were developed by Touitou et al.,1997, as additional novel lipid carriers composed of ethanol, phospholipids, and water. They are reported to improve the skin delivery of various drugs. Ethanol is an efficient permeation enhancer that is believed to act by affecting the intercellular region of the stratum corneum. Ethosomes are soft malleable vesicles composed mainly of phospholipids, ethanol, and water. These soft vesicles represent novel vesicles carriers for enhanced delivery through the skin. The size of the ethosomes vesicles can be modulated from tens of nanometers to microns.

Microneedles or Microneedle patches or Microarray patches are micron-scaled medical devices used to administer vaccines, drugs, and other therapeutic agents. While microneedles were initially explored for transdermal drug delivery applications, their use has been extended for the intraocular, vaginal, transungual, cardiac, vascular, gastrointestinal, and intracochlear delivery of drugs. Microneedles are constructed through various methods, usually involving photolithographic processes or micromolding. These methods involve etching microscopic structure into resin or silicon in order to cast microneedles. Microneedles are made from a variety of material ranging from silicon, titanium, stainless steel, and polymers. Some microneedles are made of a drug to be delivered to the body but are shaped into a needle so they will penetrate the skin. The microneedles range in size, shape, and function but are all used as an alternative to other delivery methods like the conventional hypodermic needle or other injection apparatus.
Topical drug delivery (TDD) is a route of drug administration that allows the topical formulation to be delivered across the skin upon application, hence producing a localized effect to treat skin disorders like eczema. The formulation of topical drugs can be classified into corticosteroids, antibiotics, antiseptics, and anti-fungal. The mechanism of topical delivery includes the diffusion and metabolism of drugs in the skin. Historically, topical route was the first route of medication used to deliver drugs in humans in ancient Egyptian and Babylonian in 3000 BCE. In these ancient cities, topical medications like ointments and potions were used on the skin. The delivery of topical drugs needs to pass through multiple skin layers and undergo pharmacokinetics, hence factor like dermal diseases minimize the bioavailability of the topical drugs. The wide use of topical drugs leads to the advancement in topical drug delivery. These advancements are used to enhance the delivery of topical medications to the skin by using chemical and physical agents. For chemical agents, carriers like liposomes and nanotechnologies are used to enhance the absorption of topical drugs. On the other hand, physical agents, like micro-needles is other approach for enhancement ofabsorption. Besides using carriers, other factors such as pH, lipophilicity, and drug molecule size govern the effectiveness of topical formulation.

Mark Robert Prausnitz is an American chemical engineer, currently Regents’ Professor and J. Erskine Love, Jr. Chair in Chemical & Biomolecular Engineering at the Georgia Institute of Technology, He also serves as Adjunct Professor of Biomedical Engineering at Emory University and Adjunct Professor of Chemical & Biomolecular Engineering at the Korea Advanced Institute of Science and Technology. He is known for pioneering microneedle technology for minimally invasive drug and vaccine administration, which has found applications in transdermal, ocular, oral, and sustained release delivery systems.
References
- ↑ Maher, Sam; Casettari, Luca; Illum, Lisbeth (July 2019). "Transmucosal Absorption Enhancers in the Drug Delivery Field". Pharmaceutics. 11 (7): 339. doi: 10.3390/pharmaceutics11070339 . ISSN 1999-4923. PMC 6680553 . PMID 31311173.
- ↑ Williams, Adrian C; Barry, Brian W (2004-03-27). "Penetration enhancers". Advanced Drug Delivery Reviews. Breaking the Skin Barrier. 56 (5): 603–618. doi:10.1016/j.addr.2003.10.025. ISSN 0169-409X. PMID 15019749.
- ↑ Ita, Kevin (2020-01-01), Ita, Kevin (ed.), "Chapter 5 - Chemical permeation enhancers", Transdermal Drug Delivery, Academic Press, pp. 63–96, ISBN 978-0-12-822550-9 , retrieved 2022-11-15
- ↑ Lane, Majella E. (2013-04-15). "Skin penetration enhancers". International Journal of Pharmaceutics. 447 (1): 12–21. doi:10.1016/j.ijpharm.2013.02.040. ISSN 0378-5173. PMID 23462366.
- ↑ Moiseev, Roman V.; Morrison, Peter W. J.; Steele, Fraser; Khutoryanskiy, Vitaliy V. (July 2019). "Penetration Enhancers in Ocular Drug Delivery". Pharmaceutics. 11 (7): 321. doi: 10.3390/pharmaceutics11070321 . ISSN 1999-4923. PMC 6681039 . PMID 31324063.
- ↑ Thareja, Abhinav; Hughes, Helen; Alvarez-Lorenzo, Carmen; Hakkarainen, Jenni J.; Ahmed, Zubair (February 2021). "Penetration Enhancers for Topical Drug Delivery to the Ocular Posterior Segment—A Systematic Review". Pharmaceutics. 13 (2): 276. doi: 10.3390/pharmaceutics13020276 . ISSN 1999-4923. PMC 7922526 . PMID 33670762.
- ↑ Datta, Sandipan; Baudouin, Christophe; Brignole-Baudouin, Francoise; Denoyer, Alexandre; Cortopassi, Gino A. (April 2017). "The Eye Drop Preservative Benzalkonium Chloride Potently Induces Mitochondrial Dysfunction and Preferentially Affects LHON Mutant Cells". Investigative Ophthalmology & Visual Science. 58 (4): 2406–2412. doi:10.1167/iovs.16-20903. ISSN 0146-0404. PMC 5407244 . PMID 28444329.
- ↑ Velloso, María Inés; Landoni, Fabiana (2022-03-28). "Penetration Enhancers for the Development of Intranasal Formulations for Use in Equines". International Journal of Equine Science. 1 (1): 16–32–16–32. ISSN 2805-3117.
- ↑ Rassu, Giovanna; Ferraro, Luca; Pavan, Barbara; Giunchedi, Paolo; Gavini, Elisabetta; Dalpiaz, Alessandro (December 2018). "The Role of Combined Penetration Enhancers in Nasal Microspheres on In Vivo Drug Bioavailability". Pharmaceutics. 10 (4): 206. doi: 10.3390/pharmaceutics10040206 . ISSN 1999-4923. PMC 6321492 . PMID 30373187.