Related Research Articles
Health care reform is for the most part governmental policy that affects health care delivery in a given place. Health care reform typically attempts to:

Medicare is a government national health insurance program in the United States, begun in 1965 under the Social Security Administration (SSA) and now administered by the Centers for Medicare and Medicaid Services (CMS). It primarily provides health insurance for Americans aged 65 and older, but also for some younger people with disability status as determined by the SSA, including people with end stage renal disease and amyotrophic lateral sclerosis.
An NHS trust is an organisational unit within the National Health Services of England and Wales, generally serving either a geographical area or a specialised function. In any particular location there may be several trusts involved in the different aspects of providing healthcare to the local population. As of April 2020 there were altogether 217 trusts, and they employ around 800,000 of the NHS's 1.2 million staff.
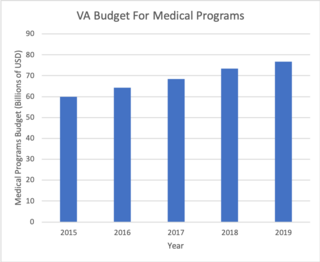
The Veterans Health Administration (VHA) is the component of the United States Department of Veterans Affairs (VA) led by the Under Secretary of Veterans Affairs for Health that implements the healthcare program of the VA through a nationalized healthcare service in the United States, providing healthcare and healthcare-adjacent services to veterans through the administration and operation of 146 VA Medical Centers (VAMC) with integrated outpatient clinics, 772 Community Based Outpatient Clinics (CBOC), and 134 VA Community Living Centers Programs. It is the largest division in the department, and second largest in the entire federal government, employing over 350,000 employees. All VA hospitals, clinics and medical centers are owned by and operated by the Department of Veterans Affairs, and all of the staff employed in VA hospitals are federal employees. Because of this, veterans that qualify for VHA healthcare do not pay premiums or deductibles for their healthcare but may have to make copayments depending on the medical procedure. VHA is not a part of the US Department of Defense Military Health System.

Preventive healthcare, or prophylaxis, is the application of healthcare measures to prevent diseases. Disease and disability are affected by environmental factors, genetic predisposition, disease agents, and lifestyle choices, and are dynamic processes that begin before individuals realize they are affected. Disease prevention relies on anticipatory actions that can be categorized as primal, primary, secondary, and tertiary prevention.
The term managed care or managed healthcare is used in the United States to describe a group of activities intended to reduce the cost of providing health care and providing American health insurance while improving the quality of that care. It has become the predominant system of delivering and receiving American health care since its implementation in the early 1980s, and has been largely unaffected by the Affordable Care Act of 2010.
...intended to reduce unnecessary health care costs through a variety of mechanisms, including: economic incentives for physicians and patients to select less costly forms of care; programs for reviewing the medical necessity of specific services; increased beneficiary cost sharing; controls on inpatient admissions and lengths of stay; the establishment of cost-sharing incentives for outpatient surgery; selective contracting with health care providers; and the intensive management of high-cost health care cases. The programs may be provided in a variety of settings, such as Health Maintenance Organizations and Preferred Provider Organizations.
Clinical governance is a systematic approach to maintaining and improving the quality of patient care within the National Health Service (NHS) and private sector health care. Clinical governance became important in health care after the Bristol heart scandal in 1995, during which an anaesthetist, Dr Stephen Bolsin, exposed the high mortality rate for paediatric cardiac surgery at the Bristol Royal Infirmary. It was originally elaborated within the United Kingdom National Health Service (NHS), and its most widely cited formal definition describes it as:
A framework through which NHS organisations are accountable for continually improving the quality of their services and safeguarding high standards of care by creating an environment in which excellence in clinical care will flourish.

The Healthcare Effectiveness Data and Information Set (HEDIS) is a widely used set of performance measures in the managed care industry, developed and maintained by the National Committee for Quality Assurance (NCQA).
In the healthcare industry, pay for performance (P4P), also known as "value-based purchasing", is a payment model that offers financial incentives to physicians, hospitals, medical groups, and other healthcare providers for meeting certain performance measures. Clinical outcomes, such as longer survival, are difficult to measure, so pay for performance systems usually evaluate process quality and efficiency, such as measuring blood pressure, lowering blood pressure, or counseling patients to stop smoking. This model also penalizes health care providers for poor outcomes, medical errors, or increased costs. Integrated delivery systems where insurers and providers share in the cost are intended to help align incentives for value-based care.
The National Health and Medical Research Council (NHMRC) is the main statutory authority of the Australian Government responsible for medical research. It was the eighth largest research funding body in the world in 2016, and NHMRC-funded research is globally recognised for its high quality. Around 45% of all Australian medical research from 2008–12 was funded by the federal government, through the NHMRC.
Patient safety is a discipline that emphasizes safety in health care through the prevention, reduction, reporting and analysis of error and other types of unnecessary harm that often lead to adverse patient events. The frequency and magnitude of avoidable adverse events, often known as patient safety incidents, experienced by patients was not well known until the 1990s, when multiple countries reported significant numbers of patients harmed and killed by medical errors. Recognizing that healthcare errors impact 1 in every 10 patients around the world, the World Health Organization (WHO) calls patient safety an endemic concern. Indeed, patient safety has emerged as a distinct healthcare discipline supported by an immature yet developing scientific framework. There is a significant transdisciplinary body of theoretical and research literature that informs the science of patient safety with mobile health apps being a growing area of research.
A Patient Safety Organization (PSO) is a group, institution, or association that improves medical care by reducing medical errors. Common functions of patient safety organizations are data collection, analysis, reporting, education, funding, and advocacy. A PSO differs from a Federally designed Patient Safety Organization (PSO), which provides health care providers in the U.S. privilege and confidentiality protections for efforts to improve patient safety and the quality of patient care delivery
The Government Performance and Results Act of 1993 (GPRA) is a United States law enacted in 1993, one of a series of laws designed to improve government performance management. The GPRA requires agencies to engage in performance management tasks such as setting goals, measuring results, and reporting their progress. In order to comply with the GPRA, agencies produce strategic plans, performance plans, and conduct gap analyses of projects. The GPRA of 1993 established project planning, strategic planning, and set up a framework of reporting for agencies to show the progress they make towards achieving their goals.
Inpatient care is the care of patients whose condition requires admission to a hospital. Progress in modern medicine and the advent of comprehensive out-patient clinics ensure that patients are only admitted to a hospital when they are extremely ill or have severe physical trauma.

The National Health Service (NHS) is the umbrella term for the publicly funded healthcare systems of the United Kingdom, comprising the National Health Service in England, NHS Scotland and NHS Wales. Health and Social Care in Northern Ireland was created separately and is often locally referred to as "the NHS". The original three systems were established in 1948 as part of major social reforms following the Second World War. The founding principles were that services should be comprehensive, universal and free at the point of delivery—a health service based on clinical need, not ability to pay. Each service provides a comprehensive range of health services, provided without charge for people ordinarily resident in the United Kingdom apart from dental treatment and optical care. In England, NHS patients have to pay prescription charges; some, such as those aged over 60, or those on certain state benefits, are exempt.
Healthcare reform in the United States has a long history. Reforms have often been proposed but have rarely been accomplished. In 2010, landmark reform was passed through two federal statutes: the Patient Protection and Affordable Care Act (PPACA), signed March 23, 2010, and the Health Care and Education Reconciliation Act of 2010, which amended the PPACA and became law on March 30, 2010.
Healthcare in the United States is largely provided by private sector healthcare facilities, and paid for by a combination of public programs, private insurance, and out-of-pocket payments. The U.S. is the only developed country without a system of universal healthcare, and a significant proportion of its population lacks health insurance.
Strategy Markup Language (StratML) is an XML-based standard vocabulary and schema for the information commonly contained in strategic and performance plans and reports. StratML Part 1 specifies the elements of strategic plans, including: mission, vision, values, goals, objectives, and stakeholders. Part 2 extends Part 1 to include the additional elements required for performance plans and reports, including stakeholder roles and performance indicators.
Health care quality is a level of value provided by any health care resource, as determined by some measurement. As with quality in other fields, it is an assessment of whether something is good enough and whether it is suitable for its purpose. The goal of health care is to provide medical resources of high quality to all who need them; that is, to ensure good quality of life, cure illnesses when possible, to extend life expectancy, and so on. Researchers use a variety of quality measures to attempt to determine health care quality, including counts of a therapy's reduction or lessening of diseases identified by medical diagnosis, a decrease in the number of risk factors which people have following preventive care, or a survey of health indicators in a population who are accessing certain kinds of care.

Healthcare in Belize is provided through both public and private healthcare systems. The Ministry of Health (MoH) is the government agency responsible for overseeing the entire health sector and is also the largest provider of public health services in Belize. The MoH offers affordable care to a majority of Belizeans with a strong focus on providing quality healthcare through a range of public programs and institutions.
References
- ↑ Strategy Markup Language (StratML) Part 2, Performance Plans and Reports, is an American national standard (ANSI/AIIM 22:2017) for performance reports.
- ↑ Section 10 of the GPRA Modernization Act (GPRAMA) requires U.S. federal agencies to publish their performance reports in machine-readable format, like StratML.
- ↑ Robert Schwartz, John Mayne (2005), Quality matters, ISBN 978-0-7658-0256-9
- ↑ A Epstein (July 6, 1995), "Performance reports on quality--prototypes, problems, and prospects", New England Journal of Medicine, 333 (1): 57–61, doi:10.1056/NEJM199507063330114, PMID 7777000