Related Research Articles

Cardiac arrest, also known as sudden cardiac arrest (SCA), is when the heart suddenly and unexpectedly stops beating. When the heart stops beating, blood cannot properly circulate around the body and the blood flow to the brain and other organs is decreased. When the brain does not receive enough blood, this can cause a person to lose consciousness and brain cells can start to die due to lack of oxygen. Coma and persistent vegetative state may result from cardiac arrest. Cardiac arrest is also identified by a lack of central pulses and abnormal or absent breathing.

Cardiopulmonary resuscitation (CPR) is an emergency procedure consisting of chest compressions often combined with artificial ventilation, or mouth to mouth in an effort to manually preserve intact brain function until further measures are taken to restore spontaneous blood circulation and breathing in a person who is in cardiac arrest. It is recommended for those who are unresponsive with no breathing or abnormal breathing, for example, agonal respirations.

Cardioversion is a medical procedure by which an abnormally fast heart rate (tachycardia) or other cardiac arrhythmia is converted to a normal rhythm using electricity or drugs. Synchronized electrical cardioversion uses a therapeutic dose of electric current to the heart at a specific moment in the cardiac cycle, restoring the activity of the electrical conduction system of the heart. Pharmacologic cardioversion, also called chemical cardioversion, uses antiarrhythmia medication instead of an electrical shock.

Advanced cardiac life support, advanced cardiovascular life support (ACLS) refers to a set of clinical guidelines established by the American Heart Association (AHA) for the urgent and emergent treatment of life-threatening cardiovascular conditions that will cause or have caused cardiac arrest, using advanced medical procedures, medications, and techniques. ACLS expands on Basic Life Support (BLS) by adding recommendations on additional medication and advanced procedure use to the CPR guidelines that are fundamental and efficacious in BLS. ACLS is practiced by advanced medical providers including physicians, some nurses and paramedics; these providers are usually required to hold certifications in ACLS care.

Defibrillation is a treatment for life-threatening cardiac arrhythmias, specifically ventricular fibrillation (V-Fib) and non-perfusing ventricular tachycardia (V-Tach). A defibrillator delivers a dose of electric current to the heart. Although not fully understood, this process depolarizes a large amount of the heart muscle, ending the arrhythmia. Subsequently, the body's natural pacemaker in the sinoatrial node of the heart is able to re-establish normal sinus rhythm. A heart which is in asystole (flatline) cannot be restarted by a defibrillator; it would be treated only by cardiopulmonary resuscitation (CPR) and medication, and then by cardioversion or defibrillation if it converts into a shockable rhythm.

Ventricular fibrillation is an abnormal heart rhythm in which the ventricles of the heart quiver. It is due to disorganized electrical activity. Ventricular fibrillation results in cardiac arrest with loss of consciousness and no pulse. This is followed by sudden cardiac death in the absence of treatment. Ventricular fibrillation is initially found in about 10% of people with cardiac arrest.

Asystole is the absence of ventricular contractions in the context of a lethal heart arrhythmia. Asystole is the most serious form of cardiac arrest and is usually irreversible. Also referred to as cardiac flatline, asystole is the state of total cessation of electrical activity from the heart, which means no tissue contraction from the heart muscle and therefore no blood flow to the rest of the body.
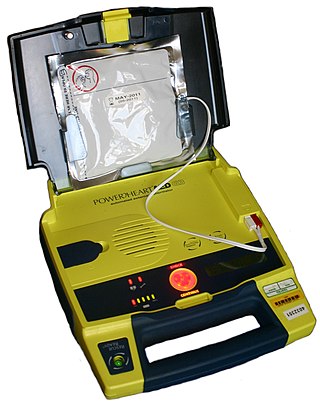
An automated external defibrillator or automatic electronic defibrillator (AED) is a portable electronic device that automatically diagnoses the life-threatening cardiac arrhythmias of ventricular fibrillation (VF) and pulseless ventricular tachycardia, and is able to treat them through defibrillation, the application of electricity which stops the arrhythmia, allowing the heart to re-establish an effective rhythm.

An implantable cardioverter-defibrillator (ICD) or automated implantable cardioverter defibrillator (AICD) is a device implantable inside the body, able to perform defibrillation, and depending on the type, cardioversion and pacing of the heart. The ICD is the first-line treatment and prophylactic therapy for patients at risk for sudden cardiac death due to ventricular fibrillation and ventricular tachycardia.
Ventricular tachycardia is a cardiovascular disorder in which fast heart rate occurs in the ventricles of the heart. Although a few seconds of VT may not result in permanent problems, longer periods are dangerous; and multiple episodes over a short period of time are referred to as an electrical storm. Short periods may occur without symptoms, or present with lightheadedness, palpitations, shortness of breath, chest pain, and decreased level of consciousness. Ventricular tachycardia may lead to coma and persistent vegetative state due to lack of blood and oxygen to the brain. Ventricular tachycardia may result in ventricular fibrillation (VF) and turn into cardiac arrest. This conversion of the VT into VF is called the degeneration of the VT. It is found initially in about 7% of people in cardiac arrest.
Pulseless electrical activity (PEA) is a form of cardiac arrest in which the electrocardiogram shows a heart rhythm that should produce a pulse, but does not. Pulseless electrical activity is found initially in about 20% of out-of-hospital cardiac arrests and about 50% of in-hospital cardiac arrests.

Advanced Life Support (ALS) is a set of life saving protocols and skills that extend basic life support to further support the circulation and provide an open airway and adequate ventilation (breathing).

ABC and its variations are initialism mnemonics for essential steps used by both medical professionals and lay persons when dealing with a patient. In its original form it stands for Airway, Breathing, and Circulation. The protocol was originally developed as a memory aid for rescuers performing cardiopulmonary resuscitation, and the most widely known use of the initialism is in the care of the unconscious or unresponsive patient, although it is also used as a reminder of the priorities for assessment and treatment of patients in many acute medical and trauma situations, from first-aid to hospital medical treatment. Airway, breathing, and circulation are all vital for life, and each is required, in that order, for the next to be effective: a viable Airway is necessary for Breathing to provide oxygenated blood for Circulation. Since its development, the mnemonic has been extended and modified to fit the different areas in which it is used, with different versions changing the meaning of letters or adding other letters.
Commotio cordis is a rare disruption of heart rhythm that occurs as a result of a blow to the area directly over the heart at a critical instant during the cycle of a heartbeat. The condition is 97% fatal if not treated within three minutes. This sudden rise in intracavitary pressure leads to disruption of normal heart electrical activity, followed instantly by ventricular fibrillation, complete disorganization of the heart's pumping function, and cardiac arrest. It is not caused by mechanical damage to the heart muscle or surrounding organs and is not the result of heart disease.
The chain of survival refers to a series of actions that, properly executed, reduce the mortality associated with sudden cardiac arrest. Like any chain, the chain of survival is only as strong as its weakest link. The six interdependent links in the chain of survival are early recognition of sudden cardiac arrest and access to emergency medical care, early CPR, early defibrillation, early advanced cardiac life support, and physical and emotional recovery. The first three links in the chain can be performed by lay bystanders, while the second three links are designated to medical professionals. Currently, between 70 and 90% of cardiac arrest patients die before they reach the hospital. However, a cardiac arrest does not have to be lethal if bystanders can take the right steps immediately.
Pediatric advanced life support (PALS) is a course offered by the American Heart Association (AHA) for health care providers who take care of children and infants in the emergency room, critical care and intensive care units in the hospital, and out of hospital. The course teaches healthcare providers how to assess injured and sick children and recognize and treat respiratory distress/failure, shock, cardiac arrest, and arrhythmias.
A wearable cardioverter defibrillator (WCD) is a non-invasive, external device for patients at risk of sudden cardiac arrest (SCA). It allows physicians time to assess their patient's arrhythmic risk and see if their ejection fraction improves before determining the next steps in patient care. It is a leased device. A summary of the device, its technology and indications was published in 2017 and reviewed by the EHRA Scientific Documents Committee.

Arrhythmias, also known as cardiac arrhythmias, are irregularities in the heartbeat, including when it is too fast or too slow. A resting heart rate that is too fast – above 100 beats per minute in adults – is called tachycardia, and a resting heart rate that is too slow – below 60 beats per minute – is called bradycardia. Some types of arrhythmias have no symptoms. Symptoms, when present, may include palpitations or feeling a pause between heartbeats. In more serious cases, there may be lightheadedness, passing out, shortness of breath, chest pain, or decreased level of consciousness. While most cases of arrhythmia are not serious, some predispose a person to complications such as stroke or heart failure. Others may result in sudden death.
Return of spontaneous circulation (ROSC) is the resumption of a sustained heart rhythm that perfuses the body after cardiac arrest. It is commonly associated with significant respiratory effort. Signs of return of spontaneous circulation include breathing, coughing, or movement and a palpable pulse or a measurable blood pressure. Someone is considered to have sustained return of spontaneous circulation when circulation persists and cardiopulmonary resuscitation has ceased for at least 20 consecutive minutes.

Rearrest is a phenomenon that involves the resumption of a lethal cardiac dysrhythmia after successful return of spontaneous circulation (ROSC) has been achieved during the course of resuscitation. Survival to hospital discharge rates are as low as 7% for cardiac arrest in general and although treatable, rearrest may worsen these survival chances. Rearrest commonly occurs in the out-of-hospital setting under the treatment of health care providers.
References
- 1 2 Neumar, RW; Shuster, M; Callaway, CW; Gent, LM; Atkins, DL; Bhanji, F; Brooks, SC; de Caen, AR; Donnino, MW; Ferrer, JM; Kleinman, ME; Kronick, SL; Lavonas, EJ; Link, MS; Mancini, ME; Morrison, LJ; O'Connor, RE; Samson, RA; Schexnayder, SM; Singletary, EM; Sinz, EH; Travers, AH; Wyckoff, MH; Hazinski, MF (3 November 2015). "Part 1: Executive Summary: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 132 (18 Suppl 2): S315-67. doi: 10.1161/cir.0000000000000252 . PMID 26472989.
- 1 2 3 Nehme, Z; Andrew, E; Bernard, SA; Smith, K (Aug 27, 2013). "Treatment of monitored out-of-hospital ventricular fibrillation and pulseless ventricular tachycardia utilizing the precordial thump". Resuscitation. 84 (12): 1691–6. doi:10.1016/j.resuscitation.2013.08.011. PMID 23994203.

- ↑ Cave, DM; Gazmuri, RJ; Otto, CW; Nadkarni, VM; Cheng, A; Brooks, SC; Daya, M; Sutton, RM; Branson, R; Hazinski, MF (Nov 2, 2010). "Part 7: CPR techniques and devices: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 122 (18 Suppl 3): S720-8. doi:10.1161/CIRCULATIONAHA.110.970970. PMC 3741663 . PMID 20956223.

- 1 2 Cotoi, S. (1981-05-01). "Precordial thump and termination of cardiac reentrant tachyarrhythmias". American Heart Journal. 101 (5): 675–677. doi:10.1016/0002-8703(81)90239-8. ISSN 0002-8703. PMID 7223609.
- 1 2 Miller, Jeffrey; Tresch, Donald; Horwitz, Louis; Thompson, Bruce M; Aprahamian, Charles; Darin, Joseph C (1984-09-01). "The precordial thump". Annals of Emergency Medicine. Cardiopulmonary-cerebral Resuscitation: State of the Art. 13 (9, Part 2): 791–794. doi:10.1016/S0196-0644(84)80439-4. ISSN 0196-0644. PMID 6476543.
- ↑ Madias, Christopher; Maron, Barry J.; Alsheikh-Ali, Alawi A.; Rajab, Mohammad; Estes, N. A. Mark; Link, Mark S. (2009-10-01). "Precordial thump for cardiac arrest is effective for asystole but not for ventricular fibrillation". Heart Rhythm. 6 (10): 1495–1500. doi:10.1016/j.hrthm.2009.06.029. ISSN 1547-5271. PMID 19968931.
- 1 2 Haman, Ludek; Parizek, Petr; Vojacek, Jan (2009-01-01). "Precordial thump efficacy in termination of induced ventricular arrhythmias". Resuscitation. 80 (1): 14–16. doi:10.1016/j.resuscitation.2008.07.022. ISSN 0300-9572. PMID 18952350.
- ↑ Dee, Ryan; Smith, Michael; et al. (2021). "The effect of alternative methods of cardiopulmonary resuscitation — Cough CPR, percussion pacing or precordial thump — on outcomes following cardiac arrest. A systematic review". Resuscitation. 162: 73–81.
- ↑ Hutchison, Julia; Hu, Eugene W. (2024). "Precordial Thump". National Library of Medicine. Retrieved 23 October 2024.
- ↑ Diehl, Digby (2000). "The Emergency Medical Services Program". To Improve Health and Health Care. Vol. 2000. Robert Wood Johnson Foundation. p. 21.
{{cite book}}:|work=ignored (help) - ↑ "Guideline 11.3: Precordial Thump & Fist Pacing" (PDF). Index of Guidelines. Australian Resuscitation Council and New Zealand Resuscitation Council. July 2011. Archived from the original on October 6, 2011. Retrieved February 15, 2014.
- ↑ Eich, C.; Bleckmann, A.; Schwarz, S. K. W. (2007). "Percussion pacing--an almost forgotten procedure for haemodynamically unstable bradycardias? A report of three case studies and review of the literature". British Journal of Anaesthesia. 98 (4): 429–433. doi: 10.1093/bja/aem007 . PMID 17327252.