Related Research Articles

Bipolar disorder, previously known as manic depression, is a mental disorder characterized by periods of depression and periods of abnormally elevated mood that last from days to weeks each. If the elevated mood is severe or associated with psychosis, it is called mania; if it is less severe, it is called hypomania. During mania, an individual behaves or feels abnormally energetic, happy or irritable, and they often make impulsive decisions with little regard for the consequences. There is usually also a reduced need for sleep during manic phases. During periods of depression, the individual may experience crying and have a negative outlook on life and poor eye contact with others. The risk of suicide is high; over a period of 20 years, 6% of those with bipolar disorder died by suicide, while 30–40% engaged in self-harm. Other mental health issues, such as anxiety disorders and substance use disorders, are commonly associated with bipolar disorder.

Cognitive behavioral therapy (CBT) is a psycho-social intervention that aims to reduce symptoms of various mental health conditions, primarily depression and anxiety disorders. CBT focuses on challenging and changing cognitive distortions and their associated behaviors to improve emotional regulation and develop personal coping strategies that target solving current problems. Though it was originally designed to treat depression, its uses have been expanded to include the treatment of many mental health conditions, including anxiety, substance use disorders, marital problems, and eating disorders. CBT includes a number of cognitive or behavioral psychotherapies that treat defined psychopathologies using evidence-based techniques and strategies.

Major depressive disorder (MDD), also known as clinical depression, is a mental disorder characterized by at least two weeks of pervasive low mood, low self-esteem, and loss of interest or pleasure in normally enjoyable activities. Introduced by a group of US clinicians in the mid-1970s, the term was adopted by the American Psychiatric Association for this symptom cluster under mood disorders in the 1980 version of the Diagnostic and Statistical Manual of Mental Disorders (DSM-III), and has become widely used since.

Psychosis is a condition of the mind that results in difficulties determining what is real and what is not real. Symptoms may include delusions and hallucinations, among other features. Additional symptoms are incoherent speech and behavior that is inappropriate for a given situation. There may also be sleep problems, social withdrawal, lack of motivation, and difficulties carrying out daily activities. Psychosis can have serious adverse outcomes.
Schizophrenia is a mental disorder characterized by continuous or relapsing episodes of psychosis. Major symptoms include hallucinations, delusions, and disorganized thinking. Other symptoms include social withdrawal, decreased emotional expression, and apathy. Symptoms typically develop gradually, begin during young adulthood, and in many cases never become resolved. There is no objective diagnostic test; diagnosis is based on observed behavior, a history that includes the person's reported experiences, and reports of others familiar with the person. To be diagnosed with schizophrenia, symptoms and functional impairment need to be present for six months (DSM-5) or one month (ICD-11). Many people with schizophrenia have other mental disorders, especially substance use disorders, depressive disorders, anxiety disorders, and obsessive–compulsive disorder.
Schizoaffective disorder is a mental disorder characterized by abnormal thought processes and an unstable mood. This diagnosis is made when the person has symptoms of both schizophrenia and a mood disorder: either bipolar disorder or depression. The main criterion for a diagnosis of schizoaffective disorder is the presence of psychotic symptoms for at least two weeks without any mood symptoms present. Schizoaffective disorder can often be misdiagnosed when the correct diagnosis may be psychotic depression, bipolar I disorder, schizophreniform disorder, or schizophrenia. It is imperative for providers to accurately diagnose patients, as treatment and prognosis differ greatly for most of these diagnoses.
Anhedonia is a diverse array of deficits in hedonic function, including reduced motivation or ability to experience pleasure. While earlier definitions emphasized the inability to experience pleasure, anhedonia is currently used by researchers to refer to reduced motivation, reduced anticipatory pleasure (wanting), reduced consummatory pleasure (liking), and deficits in reinforcement learning. In the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), anhedonia is a component of depressive disorders, substance-related disorders, psychotic disorders, and personality disorders, where it is defined by either a reduced ability to experience pleasure, or a diminished interest in engaging in pleasurable activities. While the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) does not explicitly mention anhedonia, the depressive symptom analogous to anhedonia as described in the DSM-5 is a loss of interest or pleasure.

Schizotypal personality disorder, also known as schizotypal disorder, is a Cluster A Personality disorder. DSM classification describes the disorder specifically as a personality disorder characterized by thought disorder, paranoia, a characteristic form of social anxiety, derealization, transient psychosis, and unconventional beliefs. People with this disorder feel pronounced discomfort in forming and maintaining social connections with other people, primarily due to the belief that other people harbor negative thoughts and views about them. Peculiar speech mannerisms and socially unexpected modes of dress are also characteristic. Schizotypal people may react oddly in conversations, not respond, or talk to themselves. They frequently interpret situations as being strange or having unusual meanings for them; paranormal and superstitious beliefs are common. Schizotypal people usually disagree with the suggestion their thoughts and behaviors are a 'disorder', and seek medical attention for depression or anxiety instead. Schizotypal personality disorder occurs in approximately 3% of the general population and is more commonly diagnosed in males.
Dysthymia, also known as persistent depressive disorder (PDD), is a mental and behavioral disorder, specifically a disorder primarily of mood, consisting of similar cognitive and physical problems as major depressive disorder, but with longer-lasting symptoms. The concept was used by Robert Spitzer as a replacement for the term "depressive personality" in the late 1970s.

Psychotic depression, also known as depressive psychosis, is a major depressive episode that is accompanied by psychotic symptoms. It can occur in the context of bipolar disorder or major depressive disorder. It can be difficult to distinguish from schizoaffective disorder, a diagnosis that requires the presence of psychotic symptoms for at least two weeks without any mood symptoms present. Unipolar psychotic depression requires that the psychotic features occur only during episodes of major depression. Diagnosis using the DSM-5 involves meeting the criteria for a major depressive episode, along with the criteria for "mood-congruent or mood-incongruent psychotic features" specifier.

l-Kynurenine is a metabolite of the amino acid l-tryptophan used in the production of niacin.
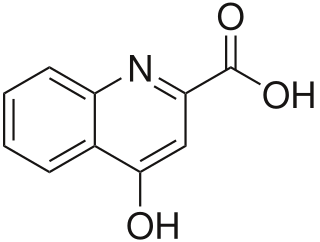
Kynurenic acid is a product of the normal metabolism of amino acid L-tryptophan. It has been shown that kynurenic acid possesses neuroactive activity. It acts as an antiexcitotoxic and anticonvulsant, most likely through acting as an antagonist at excitatory amino acid receptors. Because of this activity, it may influence important neurophysiological and neuropathological processes. As a result, kynurenic acid has been considered for use in therapy in certain neurobiological disorders. Conversely, increased levels of kynurenic acid have also been linked to certain pathological conditions.
A spectrum disorder is a mental disorder that includes a range of linked conditions, sometimes also extending to include singular symptoms and traits. The different elements of a spectrum either have a similar appearance or are thought to be caused by the same underlying mechanism. In either case, a spectrum approach is taken because there appears to be "not a unitary disorder but rather a syndrome composed of subgroups". The spectrum may represent a range of severity, comprising relatively "severe" mental disorders through to relatively "mild and nonclinical deficits".
An auditory hallucination, or paracusia, is a form of hallucination that involves perceiving sounds without auditory stimulus. While experiencing an auditory hallucination, the affected person would hear a sound or sounds which did not come from the natural environment.
Risk factors of schizophrenia include many genetic and environmental phenomena. The prevailing model of schizophrenia is that of a special neurodevelopmental disorder with no precise boundary or single cause. Schizophrenia is thought to develop from very complex gene–environment interactions with vulnerability factors. The interactions of these risk factors are intricate, as numerous and diverse medical insults from conception to adulthood can be involved. The combination of genetic and environmental factors leads to deficits in the neural circuits that affect sensory input and cognitive functions. Historically, this theory has been broadly accepted but impossible to prove given ethical limitations. The first definitive proof that schizophrenia arises from multiple biological changes in the brain was recently established in human tissue grown from patient stem cells, where the complexity of disease was found to be "even more complex than currently accepted" due to cell-by-cell encoding of schizophrenia-related neuropathology.
In medicine, a prodrome is an early sign or symptom that often indicates the onset of a disease before more diagnostically specific signs and symptoms develop. It is derived from the Greek word prodromos, meaning "running before". Prodromes may be non-specific symptoms or, in a few instances, may clearly indicate a particular disease, such as the prodromal migraine aura.
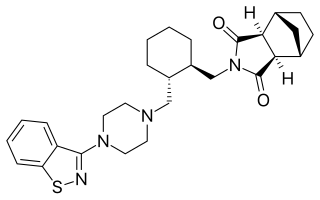
Lurasidone, sold under the trade name Latuda among others, is an antipsychotic medication used to treat schizophrenia and bipolar disorder. It is taken by mouth.
Scientific studies have found that different brain areas show altered activity in humans with major depressive disorder (MDD), and this has encouraged advocates of various theories that seek to identify a biochemical origin of the disease, as opposed to theories that emphasize psychological or situational causes. Factors spanning these causative groups include nutritional deficiencies in magnesium, vitamin D, and tryptophan with situational origin but biological impact. Several theories concerning the biologically based cause of depression have been suggested over the years, including theories revolving around monoamine neurotransmitters, neuroplasticity, neurogenesis, inflammation and the circadian rhythm. Physical illnesses, including hypothyroidism and mitochondrial disease, can also trigger depressive symptoms.
The diagnosis of schizophrenia, a psychotic disorder, is based on criteria in either the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, or the World Health Organization's International Classification of Diseases (ICD). Clinical assessment of schizophrenia is carried out by a mental health professional based on observed behavior, reported experiences, and reports of others familiar with the person. Diagnosis is usually made by a psychiatrist. Associated symptoms occur along a continuum in the population and must reach a certain severity and level of impairment before a diagnosis is made. Schizophrenia has a prevalence rate of 0.3-0.7% in the United States

Cathryn Lewis is Professor of Genetic Epidemiology and Statistics at King's College London. She is Head of Department at the Social, Genetic and Developmental Psychiatry Centre, Institute of Psychiatry, Psychology and Neuroscience.
References
- ↑ Gomez, R.G.; Posener, J.A.; Keller, J.; DeBattista, C.; Solvason, B.; Schatzberg, A.F. (Aug 2009). "Effects of major depression diagnosis and cortisol levels on indices of neurocognitive function". Psychoneuroendocrinology. 34 (7): 1012–18. doi:10.1016/j.psyneuen.2009.01.017. PMID 19261389.
- ↑ Parker, K.J.; Kenna, H.A.; Zeitzer, J.M.; Keller, J.; Blasey, C.M.; Amico, J.A.; Schatzberg A.F. (Jul 2010). "Preliminary evidence that plasma oxytocin levels are elevated in major depression". Psychiatry Res. 178 (2): 359–62. doi:10.1016/j.psychres.2009.09.017. PMC 2902664 . PMID 20494448.
- ↑ Potkin,S.G.; Macciardi, F.; Guffanti, G.; Fallon, J.H.; Wang, Q.; Turner, J.A.; Lakatos, A.; Miles, M.F.; Lander, A.; Vawter, M.P.; Xie X. (Nov 2010). "Identifying gene regulatory networks in schizophrenia". NeuroImage. 53 (3): 839–47. doi:10.1016/j.neuroimage.2010.06.036. PMC 3055795 . PMID 20600988.