Related Research Articles

An arteriovenous malformation (AVM) is an abnormal connection between arteries and veins, bypassing the capillary system. Usually congenital, this vascular anomaly is widely known because of its occurrence in the central nervous system, but can appear anywhere in the body. The symptoms of AVMs can range from none at all to intense pain or bleeding, and they can lead to other serious medical problems.

Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer in adults and is currently the most common cause of death in people with cirrhosis. HCC is the third leading cause of cancer-related deaths worldwide.
Liver tumors are abnormal growth of liver cells on or in the liver. Several distinct types of tumors can develop in the liver because the liver is made up of various cell types. Liver tumors can be classified as benign (non-cancerous) or malignant (cancerous) growths. They may be discovered on medical imaging, and the diagnosis is often confirmed with liver biopsy. Signs and symptoms of liver masses vary from being asymptomatic to patients presenting with an abdominal mass, hepatomegaly, abdominal pain, jaundice, or some other liver dysfunction. Treatment varies and is highly specific to the type of liver tumor.

Interventional radiology (IR) is a medical specialty that performs various minimally-invasive procedures using medical imaging guidance, such as x-ray fluoroscopy, computed tomography, magnetic resonance imaging, or ultrasound. IR performs both diagnostic and therapeutic procedures through very small incisions or body orifices. Diagnostic IR procedures are those intended to help make a diagnosis or guide further medical treatment, and include image-guided biopsy of a tumor or injection of an imaging contrast agent into a hollow structure, such as a blood vessel or a duct. By contrast, therapeutic IR procedures provide direct treatment—they include catheter-based medicine delivery, medical device placement, and angioplasty of narrowed structures.

A pancreaticoduodenectomy, also known as a Whipple procedure, is a major surgical operation most often performed to remove cancerous tumours from the head of the pancreas. It is also used for the treatment of pancreatic or duodenal trauma, or chronic pancreatitis. Due to the shared blood supply of organs in the proximal gastrointestinal system, surgical removal of the head of the pancreas also necessitates removal of the duodenum, proximal jejunum, gallbladder, and, occasionally, part of the stomach.
Embolization refers to the passage and lodging of an embolus within the bloodstream. It may be of natural origin (pathological), in which sense it is also called embolism, for example a pulmonary embolism; or it may be artificially induced (therapeutic), as a hemostatic treatment for bleeding or as a treatment for some types of cancer by deliberately blocking blood vessels to starve the tumor cells.
Transcatheter arterial chemoembolization (TACE) is a minimally invasive procedure performed in interventional radiology to restrict a tumor's blood supply. Small embolic particles coated with chemotherapeutic drugs are injected selectively through a catheter into an artery directly supplying the tumor. These particles both block the blood supply and induce cytotoxicity, attacking the tumor in several ways.
TheraSphere is a radiotherapy treatment for hepatocellular carcinoma (HCC) that consists of millions of microscopic, radioactive glass microspheres being infused into the arteries that feed liver tumors. These microspheres then embolize, lodging themselves in the liver's capillaries and bathing the malignancy in high levels of yttrium-90 radiation. It is currently approved as a Humanitarian Device, meaning effectiveness has not been proven, for patients as a neoadjuvant to surgery or transplantation by the U.S. Food and Drug Administration and is being used at a number of clinical centers in the United States.

Selective internal radiation therapy (SIRT), also known as transarterial radioembolization (TARE), radioembolization or intra-arterial microbrachytherapy is a form of radiation therapy used in interventional radiology to treat cancer. It is generally for selected patients with surgically unresectable cancers, especially hepatocellular carcinoma or metastasis to the liver. The treatment involves injecting tiny microspheres of radioactive material into the arteries that supply the tumor, where the spheres lodge in the small vessels of the tumor. Because this treatment combines radiotherapy with embolization, it is also called radioembolization. The chemotherapeutic analogue is called chemoembolization, of which transcatheter arterial chemoembolization (TACE) is the usual form.
Video-assisted thoracoscopic surgery (VATS) lobectomy is an approach to lung cancer surgery.

Bonnet–Dechaume–Blanc syndrome, also known as Wyburn-Mason syndrome, is a rare congenital disorder characterized by arteriovenous malformations of the brain, retina or facial nevi. The syndrome has a number of possible symptoms and can, more rarely, affect the skin, bones, kidneys, muscles, and gastrointestinal tract. When the syndrome affects the brain, people can experience severe headaches, seizures, acute stroke, meningism, and progressive neurological deficits due to acute or chronic ischaemia caused by arteriovenous shunting.
Irreversible electroporation is a soft tissue ablation technique using short but strong electrical fields to create permanent and hence lethal nanopores in the cell membrane, to disrupt cellular homeostasis. The resulting cell death results from induced apoptosis or necrosis induced by either membrane disruption or secondary breakdown of the membrane due to transmembrane transfer of electrolytes and adenosine triphosphate. The main use of IRE lies in tumor ablation in regions where precision and conservation of the extracellular matrix, blood flow and nerves are of importance. The first generation of IRE for clinical use, in the form of the NanoKnife System, became commercially available for research purposes in 2009, solely for the surgical ablation of soft tissue tumors. Cancerous tissue ablation via IRE appears to show significant cancer specific immunological responses which are currently being evaluated alone and in combination with cancer immunotherapy.
Hepatic artery embolization, also known as trans-arterial embolization (TAE), is one of the several therapeutic methods to treat primary liver tumors or metastases to the liver. The embolization therapy can reduce the size of the tumor, and decrease the tumor's impact such its hormone production, effectively decreasing symptoms. The treatment was initially developed in the early 1970s. The several types of hepatic artery treatments are based on the observation that tumor cells get nearly all their nutrients from the hepatic artery, while the normal cells of the liver get about 70-80 percent of their nutrients and 50% their oxygen supply from the portal vein, and thus can survive with the hepatic artery effectively blocked. In practice, hepatic artery embolization occludes the blood flow to the tumors, achieving significant tumor shrinkage in over 80% of people. Shrinkage rates vary.
Interventional oncology is a subspecialty field of interventional radiology that deals with the diagnosis and treatment of cancer and cancer-related problems using targeted minimally invasive procedures performed under image guidance. Interventional oncology has developed to a separate pillar of modern oncology and it employs X-ray, ultrasound, computed tomography (CT) or magnetic resonance imaging (MRI) to help guide miniaturized instruments to allow targeted and precise treatment of solid tumours located in various organs of the human body, including but not limited to the liver, kidneys, lungs, and bones. Interventional oncology treatments are routinely carried out by interventional radiologists in appropriate settings and facilities.

Prostatic artery embolization is a non-surgical technique for treatment of benign prostatic hypertrophy (BPH).

In human anatomy, the Cantlie line or Cantlie's line is an imaginary division of the liver. The division divides the liver into two planes, extending from the middle hepatic vein to the middle of the gallbladder. It is useful for performing hepatectomies.
Portal vein embolization (PVE) is a preoperative procedure performed in interventional radiology to initiate hypertrophy of the anticipated future liver remnant a couple weeks prior to a major liver resection procedure. The procedure involves injecting the right or left portal vein with embolic material to occlude portal blood flow. By occluding the blood flow to areas of the liver that will be resected away, the blood is diverted to healthy parts of the liver and induces hyperplasia. This may allow for a more extensive resection or stage bilateral resections that would otherwise be contraindicated resulting in better oncological treatment outcomes.

A liver segment is one of eight segments of the liver as described in the widely used Couinaud classification in the anatomy of the liver. This system divides the lobes of the liver into eight segments based on a transverse plane through the bifurcation of the main portal vein, arranged in a clockwise manner starting from the caudate lobe.
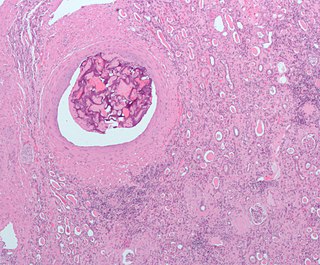
Transarterial bland embolization is a catheter-based tumor treatment of the liver. In this procedure, a variety of embolizing agents can be delivered through the tumor’s feeding artery in order to completely occlude the tumor’s blood supply. The anti-tumor effects are solely based on tumor ischemia and infarction of tumor tissue, as no chemotherapeutic agents are administered. The rationale for the use of bland embolization for hepatocellular carcinoma(HCC) and/or other hyper-vascular tumors is based on the fact that normal liver receives a dual blood supply from the hepatic artery (25%) and the portal vein (75%). As the tumor grows, it becomes increasingly dependent on the hepatic artery for blood supply. Once a tumor nodule reaches a diameter of 2 cm or more, most of the blood supply is derived from the hepatic artery. Therefore, bland embolization and transarterial chemoembolization (TACE) consist of the selective angiographic occlusion of the tumor arterial blood supply with a variety of embolizing agents, with or without the precedence of local chemotherapy infusion. The occlusion by embolic particles results in tumor hypoxia and necrosis, without affecting the normal hepatic parenchyma.

Liver angiosarcoma also known as angiosarcoma of the liver or hepatic angiosarcoma is a rare and rapidly fatal cancer arising from endothelial that line the blood vessels of the liver. It is a type of angiosarcoma. Although very rare with around 200 cases diagnosed each year, it is still considered the third most common primary liver cancer, making up around 2% of all primary liver cancers. Liver angiosarcoma can be primary, meaning it arose in the liver, or secondary, meaning the angiosarcoma arose elsewhere and metastasized to the liver. This article covers PHA, however much is also applicable to secondary tumors.
References
- ↑ Garcea, G.; Ong, S.L.; Maddern, G.J. (2009). "Predicting liver failure following major hepatectomy". Digestive and Liver Disease. 41 (11): 798–806. doi:10.1016/j.dld.2009.01.015. PMID 19303376.
- 1 2 3 Vouche, Michael; Lewandowski, Robert J.; Atassi, Rohi; Memon, Khairuddin; Gates, Vanessa L.; Ryu, Robert K.; Gaba, Ron C.; Mulcahy, Mary F.; Baker, Talia (November 2013). "Radiation lobectomy: Time-dependent analysis of future liver remnant volume in unresectable liver cancer as a bridge to resection". Journal of Hepatology. 59 (5): 1029–1036. doi:10.1016/j.jhep.2013.06.015. PMC 5085290 . PMID 23811303.
- ↑ Gaba, RC; Carroll, JJ; Carrillo, TC (2011). "Chemoembolic lobectomy: imaging findings of hepatic lobar volume reduction after transcatheter arterial chemoembolization". Diagnostic Interv Radiol. 17 (2): 177–180. doi:10.4261/1305-3825.DIR.3166-09.1. PMID 20683817.
- 1 2 3 Lewandowski, Robert J.; Donahue, Larry; Chokechanachaisakul, Attasit; Kulik, Laura; Mouli, Samdeep; Caicedo, Juan; Abecassis, Michael; Fryer, Jonathan; Salem, Riad (2016-07-01). "90Y radiation lobectomy: Outcomes following surgical resection in patients with hepatic tumors and small future liver remnant volumes". Journal of Surgical Oncology. 114 (1): 99–105. doi:10.1002/jso.24269. ISSN 1096-9098. PMID 27103352. S2CID 42996741.
- ↑ Fernández-Ros, Nerea; Silva, Nuno; Bilbao, Jose Ignacio; Iñarrairaegui, Mercedes; Benito, Alberto; D'Avola, Delia; Rodriguez, Macarena; Rotellar, Fernando; Pardo, Fernando (March 2014). "Partial liver volume radioembolization induces hypertrophy in the spared hemiliver and no major signs of portal hypertension". HPB. 16 (3): 243–249. doi:10.1111/hpb.12095. PMC 3945850 . PMID 23530966.
- ↑ Shah, Jehan L.; Zendejas-Ruiz, Ivan R.; Thornton, Linday M.; Geller, Brian S.; Grajo, Joseph R.; Collinsworth, Amy; George Jr, Thomas J.; Toskich, Beau (2017-12-04). "Neoadjuvant transarterial radiation lobectomy for colorectal hepatic metastases: a small cohort analysis on safety, efficacy, and radiopathologic correlation". Journal of Gastrointestinal Oncology. 8 (3): E43–E51. doi: 10.21037/jgo.2017.01.26 . ISSN 2219-679X. PMC 5506271 . PMID 28736649.
- ↑ Madoff, David C.; Vauthey, Jean-Nicolas (2013-06-01). "Re: Portal Vein Embolization: What Do We Know?". CardioVascular and Interventional Radiology. 36 (3): 870–871. doi:10.1007/s00270-012-0407-z. ISSN 0174-1551. PMID 22584753. S2CID 43947.
- ↑ Lienden, K. P. van; Esschert, J. W. van den; Graaf, W. de; Bipat, S.; Lameris, J. S.; Gulik, T. M. van; Delden, O. M. van (2013-02-01). "Portal Vein Embolization Before Liver Resection: A Systematic Review". CardioVascular and Interventional Radiology. 36 (1): 25–34. doi:10.1007/s00270-012-0440-y. ISSN 0174-1551. PMC 3549243 . PMID 22806245.
- ↑ Simoneau, Eve; Aljiffry, Murad; Salman, Ayat; Abualhassan, Nasser; Cabrera, Tatiana; Valenti, David; Baage, Arwa El; Jamal, Mohammad; Kavan, Petr (July 2012). "Portal vein embolization stimulates tumour growth in patients with colorectal cancer liver metastases". HPB. 14 (7): 461–468. doi:10.1111/j.1477-2574.2012.00476.x. PMC 3384876 . PMID 22672548.
- 1 2 3 Kandarpa, K; Machan, L (2012). Handbook of Interventional Radiologic Procedures (4td ed.). LWW.
- 1 2 Riaz, Ahsun; Awais, Rafia; Salem, Riad (2014). "Side Effects of Yttrium-90 Radioembolization". Frontiers in Oncology. 4: 198. doi: 10.3389/fonc.2014.00198 . ISSN 2234-943X. PMC 4114299 . PMID 25120955.