Related Research Articles

Electrocardiography is the process of producing an electrocardiogram. It is a graph of voltage versus time of the electrical activity of the heart using electrodes placed on the skin. These electrodes detect the small electrical changes that are a consequence of cardiac muscle depolarization followed by repolarization during each cardiac cycle (heartbeat). Changes in the normal ECG pattern occur in numerous cardiac abnormalities, including cardiac rhythm disturbances, inadequate coronary artery blood flow, and electrolyte disturbances.

Tachycardia, also called tachyarrhythmia, is a heart rate that exceeds the normal resting rate. In general, a resting heart rate over 100 beats per minute is accepted as tachycardia in adults. Heart rates above the resting rate may be normal or abnormal.
Wolff–Parkinson–White syndrome (WPWS) is a disorder due to a specific type of problem with the electrical system of the heart which has resulted in symptoms. About 40% of people with the electrical problem never develop symptoms. Symptoms can include an abnormally fast heartbeat, palpitations, shortness of breath, lightheadedness, or syncope. Rarely, cardiac arrest may occur. The most common type of irregular heartbeat that occurs is known as paroxysmal supraventricular tachycardia.

The atrioventricular node or AV node is a part of the electrical conduction system of the heart that coordinates the top of the heart. It electrically connects the atria and ventricles. The AV node lies at the lower back section of the interatrial septum near the opening of the coronary sinus, and conducts the normal electrical impulse from the atria to the ventricles. The AV node is quite compact.

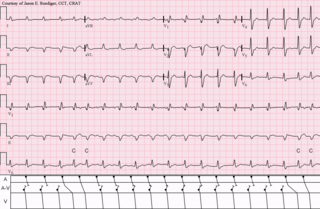
Atrial flutter (AFL) is a common abnormal heart rhythm that starts in the atrial chambers of the heart. When it first occurs, it is usually associated with a fast heart rate and is classified as a type of supraventricular tachycardia. Atrial flutter is characterized by a sudden-onset (usually) regular abnormal heart rhythm on an electrocardiogram (ECG) in which the heart rate is fast. Symptoms may include a feeling of the heart beating too fast, too hard, or skipping beats, chest discomfort, difficulty breathing, a feeling as if one's stomach has dropped, a feeling of being light-headed, or loss of consciousness.
Ventricular tachycardia is a type of regular, fast heart rate that arises from improper electrical activity in the ventricles of the heart. Although a few seconds may not result in problems, longer periods are dangerous. Short periods may occur without symptoms, or present with lightheadedness, palpitations, or chest pain. Ventricular tachycardia may result in ventricular fibrillation and turn into sudden death. It is found initially in about 7% of people in cardiac arrest.

Supraventricular tachycardia (SVT) is an abnormally fast heart rhythm arising from improper electrical activity in the upper part of the heart. There are four main types: atrial fibrillation, paroxysmal supraventricular tachycardia (PSVT), atrial flutter, and Wolff–Parkinson–White syndrome. Symptoms may include palpitations, feeling faint, sweating, shortness of breath, or chest pain.

AV-nodal reentrant tachycardia (AVNRT) is a type of abnormal fast heart rhythm. It is a type of supraventricular tachycardia (SVT), meaning that it originates from a location within the heart above the bundle of His. AV nodal reentrant tachycardia is the most common regular supraventricular tachycardia. It is more common in women than men. The main symptom is palpitations. Treatment may be with specific physical maneuvers, medications, or, rarely, synchronized cardioversion. Frequent attacks may require radiofrequency ablation, in which the abnormally conducting tissue in the heart is destroyed.

Ebstein's anomaly is a congenital heart defect in which the septal and posterior leaflets of the tricuspid valve are displaced towards the apex of the right ventricle of the heart. It is classified as a critical congenital heart defect accounting for <1% of all congenital heart defects presenting in ≈1 per 200,000 live births.
Lown–Ganong–Levine syndrome (LGL) is a pre-excitation syndrome of the heart. Those with LGL syndrome have episodes of abnormal heart racing with a short PR interval and normal QRS complexes seen on their electrocardiogram when in a normal sinus rhythm. LGL syndrome was originally thought to be due to an abnormal electrical connection between the atria and the ventricles, but is now thought to be due to accelerated conduction through the atrioventricular node in the majority of cases. The syndrome is named after Bernard Lown, William Francis Ganong, Jr., and Samuel A. Levine.

Lorcainide is a Class 1c antiarrhythmic agent that is used to help restore normal heart rhythm and conduction in patients with premature ventricular contractions, ventricular tachycardiac and Wolff-Parkinson-White syndrome. Lorcainide was developed by Janssen Pharmaceutica (Belgium) in 1968 under the commercial name Remivox and is designated by code numbers R-15889 or Ro 13-1042/001. It has a half-life of 8.9 +- 2.3 hrs which may be prolonged to 66 hrs in people with cardiac disease.
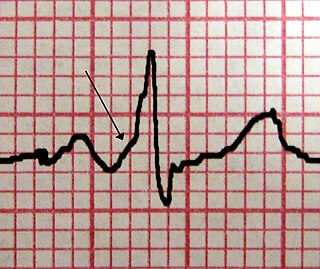
An accessory pathway is an additional electrical connection between two parts of the heart. These pathways can lead to abnormal heart rhythms or arrhythmias associated with symptoms of palpitations. Some pathways may activate a region of ventricular muscle earlier than would normally occur, referred to as pre-excitation, and this may be seen on an electrocardiogram. The combination of an accessory pathway that causes pre-excitation with arrhythmias is known as Wolff-Parkinson-White syndrome.

Junctional tachycardia is a form of supraventricular tachycardia characterized by involvement of the AV node. It can be contrasted to atrial tachycardia. It is a tachycardia associated with the generation of impulses in a focus in the region of the atrioventricular node due to an A-V disassociation. In general, the AV junction's intrinsic rate is 40-60 bpm so an accelerated junctional rhythm is from 60-100bpm and then becomes junctional tachycardia at a rate of >100 bpm.

Junctional ectopic tachycardia (JET) is a rare syndrome of the heart that manifests in patients recovering from heart surgery. It is characterized by cardiac arrhythmia, or irregular beating of the heart, caused by abnormal conduction from or through the atrioventricular node. In newborns and infants up to 6 weeks old, the disease may also be referred to as His bundle tachycardia or congenital JET.

Atrioventricular reentrant tachycardia (AVRT), or atrioventricular reciprocating tachycardia, is a type of abnormal fast heart rhythm and is classified as a type of supraventricular tachycardia (SVT). AVRT is most commonly associated with Wolff–Parkinson–White syndrome, but is also seen in permanent junctional reentrant tachycardia (PJRT). In AVRT, an accessory pathway allows electrical signals from the heart's ventricles to enter the atria and cause earlier than normal contraction, which leads to repeated stimulation of the atrioventricular node.

Arrhythmia, also known as cardiac arrhythmia or heart arrhythmia, is a group of conditions in which the heartbeat is irregular, too fast, or too slow. The heart rate that is too fast – above 100 beats per minute in adults – is called tachycardia, and a heart rate that is too slow – below 60 beats per minute – is called bradycardia. Some types of arrhythmias have no symptoms. Symptoms, when present, may include palpitations or feeling a pause between heartbeats. In more serious cases, there may be lightheadedness, passing out, shortness of breath or chest pain. While most types of arrhythmia are not serious, some predispose a person to complications such as stroke or heart failure. Others may result in sudden death.

Permanent junctional reciprocating tachycardia(PJRT) is a rare cardiac arrhythmia. It is a supraventricular tachycardia, and a cause of atrioventricular reentrant tachycardia (AVRT). PJRT can cause chronic tachycardia that, untreated, leads to cardiomyopathy. The cause is an accessory pathway in the heart which conducts from the ventricles back to the atria. Unlike the accessory pathway in a more common cause of AVRT, Wolff-Parkinson-White syndrome, the accessory pathway in PJRT conducts slowly. This means that the associated tachycardia may be subclinical and only diagnosed at a late stage, after significant damage to the heart has been caused from prolonged and recurrent episodes of AVRT.

Bigeminy is a cardiac arrythmia in which there is a single ectopic beat, or irregular heartbeat, following each regular heartbeat. Most often this is due to ectopic beats occurring so frequently that there is one after each sinus beat, or normal heartbeat. The two beats are figuratively similar to two twins. For example, in ventricular bigeminy, a sinus beat is shortly followed by a PVC, a pause, another normal beat, and then another PVC. In atrial bigeminy, the other "twin" is a premature atrial contraction (PAC).
An automatic tachycardia is a cardiac arrhythmia which involves an area of the heart generating an abnormally fast rhythm, sometimes also called enhanced automaticity. These tachycardias, or fast heart rhythms, differ from reentrant tachycardias in which there is an abnormal electrical pathway which gives rise to the pathology. Most automatic tachycardias are supraventricular tachycardias (SVT). It is important to recognise an automatic tachycardia because the treatment will be different to that for a reentrant tachycardia. The most useful clue will be the presence of 'warm up' and 'cool down'. This means that whereas a reentrant tachycardia will both begin and end abruptly as cardiac conduction utilises then ceases to utilise the accessory pathway, an automatic tachycardia will rise and fall gradually in rate as the automatic focus increases and decreases its automatic rate of electrical discharge.
References
- ↑ "Cardiac Arrhythmias" . Retrieved 2007-07-21.
- 1 2 Am J Cardiol. 1984 Jul 30;54(2):1A-6A.
- ↑ Cardiovascular Physiology & Anesthesia. Morgan, Jr. GE, Mikhail MS, Murray MJ. Chapter 19. Clinical Anesthesiology. 4th ed. New York: McGraw-Hill; 2006.
- 1 2 Hurst's The Heart, 13e.(2011). Chapter 41. Supraventricular Tachycardia: Atrioventricular Nodal Reentry and Wolff-Parkinson-White Syndrome.
- ↑ Goodman & Gilman's The Pharmacological Basis of Therapeutics. 12th ed. |Sampson KJ, Kass RS. Chapter 29. Anti-Arrhythmic Drugs.
- ↑ Hurst's The Heart, Chapter 38. Mechanisms of Cardiac Arrhythmias and Conduction Disturbances. In V. Fuster, R.A. Walsh, R.A. Harrington (Eds)