Related Research Articles

A disease is a particular abnormal condition that adversely affects the structure or function of all or part of an organism and is not immediately due to any external injury. Diseases are often known to be medical conditions that are associated with specific signs and symptoms. A disease may be caused by external factors such as pathogens or by internal dysfunctions. For example, internal dysfunctions of the immune system can produce a variety of different diseases, including various forms of immunodeficiency, hypersensitivity, allergies, and autoimmune disorders.
Neuromyotonia (NMT) is a form of peripheral nerve hyperexcitability that causes spontaneous muscular activity resulting from repetitive motor unit action potentials of peripheral origin. NMT along with Morvan's syndrome are the most severe types in the Peripheral Nerve Hyperexciteability spectrum. Example of two more common and less severe syndromes in the spectrum are cramp fasciculation syndrome and benign fasciculation syndrome. NMT can have both hereditary and acquired (non-inherited) forms. The prevalence of NMT is unknown.
Schizoaffective disorder is a mental disorder characterized by symptoms of both schizophrenia (psychosis) and a mood disorder - either bipolar disorder or depression. The main diagnostic criterion is the presence of psychotic symptoms for at least two weeks without prominent mood symptoms. Common symptoms include hallucinations, delusions, disorganized speech and thinking, as well as mood episodes. Schizoaffective disorder can often be misdiagnosed when the correct diagnosis may be psychotic depression, bipolar I disorder, schizophreniform disorder, or schizophrenia. This is a problem as treatment and prognosis differ greatly for most of these diagnoses. Many people with schizoaffective disorder have other mental disorders including anxiety disorders.

Signs and symptoms are the observed or detectable signs, and experienced symptoms of an illness, injury, or condition.
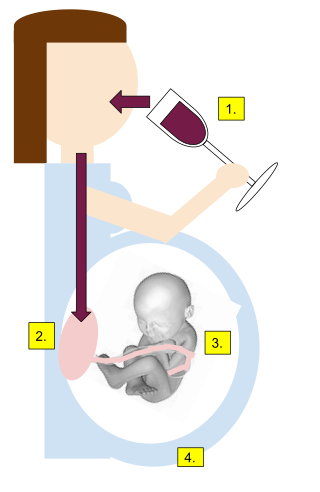
Alcohol dependence is a previous psychiatric diagnosis in which an individual is physically or psychologically dependent upon alcohol.
Pervasive developmental disorder not otherwise specified (PDD-NOS) is a historic psychiatric diagnosis first defined in 1980 that has since been incorporated into autism spectrum disorder in the DSM-5 (2013).

Granulomatosis with polyangiitis (GPA), previously known as Wegener's granulomatosis (WG), after the German physician Friedrich Wegener, is a rare long-term systemic disorder that involves the formation of granulomas and inflammation of blood vessels (vasculitis). It is an autoimmune disease and a form of vasculitis that affects small- and medium-size vessels in many organs but most commonly affects the upper respiratory tract, lungs and kidneys. The signs and symptoms of GPA are highly varied and reflect which organs are supplied by the affected blood vessels. Typical signs and symptoms include nosebleeds, stuffy nose and crustiness of nasal secretions, and inflammation of the uveal layer of the eye. Damage to the heart, lungs and kidneys can be fatal.
Clinical endpoints or clinical outcomes are outcome measures referring to occurrence of disease, symptom, sign or laboratory abnormality constituting a target outcome in clinical research trials. The term may also refer to any disease or sign that strongly motivates withdrawal of an individual or entity from the trial, then often termed a humane (clinical) endpoint.
Hypogammaglobulinemia is an immune system disorder in which not enough gamma globulins are produced in the blood. This results in a lower antibody count, which impairs the immune system, increasing risk of infection. Hypogammaglobulinemia may result from a variety of primary genetic immune system defects, such as common variable immunodeficiency, or it may be caused by secondary effects such as medication, blood cancer, or poor nutrition, or loss of gamma globulins in urine, as in nonselective glomerular proteinuria. Patients with hypogammaglobulinemia have reduced immune function; important considerations include avoiding use of live vaccines, and take precautionary measures when traveling to regions with endemic disease or poor sanitation such as receiving immunizations, taking antibiotics abroad, drinking only safe or boiled water, arranging appropriate medical cover in advance of travel, and ensuring continuation of any immunoglobulin infusions needed.

Acute myeloid leukemia (AML) is a cancer of the myeloid line of blood cells, characterized by the rapid growth of abnormal cells that build up in the bone marrow and blood and interfere with normal blood cell production. Symptoms may include feeling tired, shortness of breath, easy bruising and bleeding, and increased risk of infection. Occasionally, spread may occur to the brain, skin, or gums. As an acute leukemia, AML progresses rapidly, and is typically fatal within weeks or months if left untreated.
Juvenile myelomonocytic leukemia (JMML) is a rare form of chronic leukemia that affects children, commonly those aged four and younger. The name JMML now encompasses all diagnoses formerly referred to as juvenile chronic myeloid leukemia (JCML), chronic myelomonocytic leukemia of infancy, and infantile monosomy 7 syndrome. The average age of patients at diagnosis is two (2) years old. The World Health Organization has included JMML as a subcategory of myelodysplastic and myeloproliferative disorders.
Bipolar II disorder (BP-II) is a mood disorder on the bipolar spectrum, characterized by at least one episode of hypomania and at least one episode of major depression. Diagnosis for BP-II requires that the individual must never have experienced a full manic episode. Otherwise, one manic episode meets the criteria for bipolar I disorder (BP-I).

Acute megakaryoblastic leukemia (AMKL) is life-threatening leukemia in which malignant megakaryoblasts proliferate abnormally and injure various tissues. Megakaryoblasts are the most immature precursor cells in a platelet-forming lineage; they mature to promegakaryocytes and, ultimately, megakaryocytes which cells shed membrane-enclosed particles, i.e. platelets, into the circulation. Platelets are critical for the normal clotting of blood. While malignant megakaryoblasts usually are the predominant proliferating and tissue-damaging cells, their similarly malignant descendants, promegakaryocytes and megakaryocytes, are variable contributors to the malignancy.
A cure is a substance or procedure that ends a medical condition, such as a medication, a surgical operation, a change in lifestyle or even a philosophical mindset that helps end a person's sufferings; or the state of being healed, or cured. The medical condition could be a disease, mental illness, genetic disorder, or simply a condition a person considers socially undesirable, such as baldness or lack of breast tissue.

Clinical descriptions of ME/CFS vary. Different groups have produced sets of diagnostic criteria that share many similarities. The biggest differences between criteria are whether post-exertional malaise (PEM) is required, and the number of symptoms needed.
Brief psychotic disorder—according to the classifications of mental disorders DSM-IV-TR and DSM-5—is a psychotic condition involving the sudden onset of at least one psychotic symptom lasting 1 day to 1 month, often accompanied by emotional turmoil. Remission of all symptoms is complete with patients returning to the previous level of functioning. It may follow a period of extreme stress including the loss of a loved one. Most patients with this condition under DSM-5 would be classified as having acute and transient psychotic disorders under ICD-10. Prior to DSM-IV, this condition was called "brief reactive psychosis." This condition may or may not be recurrent, and it should not be caused by another condition.

Medical diagnosis is the process of determining which disease or condition explains a person's symptoms and signs. It is most often referred to as a diagnosis with the medical context being implicit. The information required for a diagnosis is typically collected from a history and physical examination of the person seeking medical care. Often, one or more diagnostic procedures, such as medical tests, are also done during the process. Sometimes the posthumous diagnosis is considered a kind of medical diagnosis.

Current standards for diagnosing multiple sclerosis (MS) are based on the 2018 revision of McDonald criteria. They rely on MRI detection of demyelinating lesions in the CNS, which are distributed in space (DIS) and in time (DIT). It is also a requirement that any possible known disease that produces demyelinating lesions is ruled out before applying McDonald's criteria.
Bouffée délirante (BD) is an acute and transient psychotic disorder. It is a uniquely French psychiatric diagnostic term with a long history in France and various French speaking nations: Caribbean, e.g., Haiti, Guadeloupe, Antilles and Francophone Africa. The term BD was originally coined and described by Valentin Magnan (1835–1916), fell into relative disuse and was later revived by Henri Ey (1900–1977).

Idiopathic multicentric Castleman disease (iMCD) is a subtype of Castleman disease (also known as giant lymph node hyperplasia, lymphoid hamartoma, or angiofollicular lymph node hyperplasia), a group of lymphoproliferative disorders characterized by lymph node enlargement, characteristic features on microscopic analysis of enlarged lymph node tissue, and a range of symptoms and clinical findings.
References
- ↑ "What Does Cancer Remission Really Mean?". WebMD. Retrieved 2019-06-22.
- ↑ "Definitions of the word 'remission'". Medical Dictionary. TheFreeDictionary.com. Archived from the original on 30 May 2019.
- ↑ WebMD, LLC. (2018). Martin, Laura J. (ed.). "Remission: What Does It Mean?". WebMD.com . Archived from the original on 6 April 2019.
- ↑ "What is "Cure"?". mskcc.org. Memorial Sloan Kettering Cancer Center. Archived from the original on 30 May 2019.