Related Research Articles

First aid is the first and immediate assistance given to any person with a medical emergency, with care provided to preserve life, prevent the condition from worsening, or to promote recovery until medical services arrive. First aid is generally performed by someone with basic medical or first response training. Mental health first aid is an extension of the concept of first aid to cover mental health, while psychological first aid is used as early treatment of people who are at risk for developing PTSD. Conflict first aid, focused on preservation and recovery of an individual's social or relationship well-being, is being piloted in Canada.

Diabetic ketoacidosis (DKA) is a potentially life-threatening complication of diabetes mellitus. Signs and symptoms may include vomiting, abdominal pain, deep gasping breathing, increased urination, weakness, confusion and occasionally loss of consciousness. A person's breath may develop a specific "fruity" smell. The onset of symptoms is usually rapid. People without a previous diagnosis of diabetes may develop DKA as the first obvious symptom.

Whiplash, whose formal term is whiplash associated disorders (WAD), is a range of injuries to the neck caused by or related to a sudden distortion of the neck associated with extension, although the exact injury mechanisms remain unknown. The term "whiplash" is a colloquialism. "Cervical acceleration–deceleration" (CAD) describes the mechanism of the injury, while WAD describes the subsequent injuries and symptoms.

Septic shock is a potentially fatal medical condition that occurs when sepsis, which is organ injury or damage in response to infection, leads to dangerously low blood pressure and abnormalities in cellular metabolism. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) defines septic shock as a subset of sepsis in which particularly profound circulatory, cellular, and metabolic abnormalities are associated with a greater risk of mortality than with sepsis alone. Patients with septic shock can be clinically identified by requiring a vasopressor to maintain a mean arterial pressure of 65 mm Hg or greater and having serum lactate level greater than 2 mmol/L (>18 mg/dL) in the absence of hypovolemia. This combination is associated with hospital mortality rates greater than 40%.

Digital rectal examination (DRE), also known as a prostate exam, is an internal examination of the rectum performed by a healthcare provider.
Basic life support (BLS) is a level of medical care which is used for patients with life-threatening condition of cardiac arrest until they can be given full medical care by advanced life support providers. It can be provided by trained medical personnel, such as emergency medical technicians, qualified bystanders and anybody who is trained for providing BLS and/or ACLS.

Raynaud syndrome, also known as Raynaud's phenomenon, is a medical condition in which the spasm of small arteries causes episodes of reduced blood flow to end arterioles. Typically the fingers, and, less commonly, the toes, are involved. Rarely, the nose, ears, nipples, or lips are affected. The episodes classically result in the affected part turning white and then blue. Often, numbness or pain occurs. As blood flow returns, the area turns red and burns. The episodes typically last minutes but can last several hours. The condition is named after the physician Auguste Gabriel Maurice Raynaud, who first described it in his doctoral thesis in 1862.
Hemicorporectomy is a radical surgery in which the body below the waist is amputated, transecting the lumbar spine. This removes the legs, the genitalia, urinary system, pelvic bones, anus, and rectum. It is a major procedure recommended only as a last resort for people with severe and potentially fatal illnesses such as osteomyelitis, tumors, severe traumas and intractable decubiti in, or around, the pelvis. By 2009, 66 cases had been reported in medical literature.

Airway management includes a set of maneuvers and medical procedures performed to prevent and relieve airway obstruction. This ensures an open pathway for gas exchange between a patient's lungs and the atmosphere. This is accomplished by either clearing a previously obstructed airway; or by preventing airway obstruction in cases such as anaphylaxis, the obtunded patient, or medical sedation. Airway obstruction can be caused by the tongue, foreign objects, the tissues of the airway itself, and bodily fluids such as blood and gastric contents (aspiration).
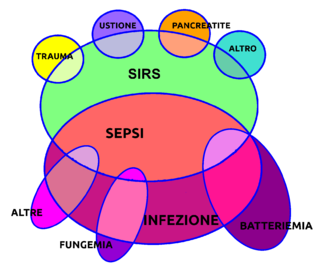
In immunology, systemic inflammatory response syndrome (SIRS) is an inflammatory state affecting the whole body. It is the body's response to an infectious or noninfectious insult. Although the definition of SIRS refers to it as an "inflammatory" response, it actually has pro- and anti-inflammatory components.
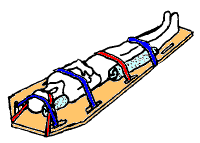
A spinal board, is a patient handling device used primarily in pre-hospital trauma care. It is designed to provide rigid support during movement of a person with suspected spinal or limb injuries. They are most commonly used by ambulance staff, as well as lifeguards and ski patrollers. Historically, backboards were also used in an attempt to "improve the posture" of young people, especially girls.

A vacuum mattress, or vacmat, is a medical device used for the immobilisation of patients, especially in case of a vertebra, pelvis or limb trauma. It is also used for manual transportation of patients for short distances. It was invented by Loed and Haederlé, who called it "shell" mattress.

In medicine, the Ottawa ankle rules are a set of guidelines for clinicians to help decide if a patient with foot or ankle pain should be offered X-rays to diagnose a possible bone fracture. Before the introduction of the rules most patients with ankle injuries would have been imaged. However the vast majority of patients with unclear ankle injuries do not have bone fractures. As a result, many unnecessary X-rays were taken, which was costly, time-consuming and a slight health risk due to radiation exposure.

ABC and its variations are initialism mnemonics for essential steps used by both medical professionals and lay persons when dealing with a patient. In its original form it stands for Airway, Breathing, and Circulation. The protocol was originally developed as a memory aid for rescuers performing cardiopulmonary resuscitation, and the most widely known use of the initialism is in the care of the unconscious or unresponsive patient, although it is also used as a reminder of the priorities for assessment and treatment of patients in many acute medical and trauma situations, from first-aid to hospital medical treatment. Airway, breathing, and circulation are all vital for life, and each is required, in that order, for the next to be effective: a viable Airway is necessary for Breathing to provide oxygenated blood for Circulation. Since its development, the mnemonic has been extended and modified to fit the different areas in which it is used, with different versions changing the meaning of letters or adding other letters.

Blunt trauma, also known as blunt force trauma or non-penetrating trauma, describes a physical trauma due to a forceful impact without penetration of the body's surface. Blunt trauma stands in contrast with penetrating trauma, which occurs when an object pierces the skin, enters body tissue, and creates an open wound. Blunt trauma occurs due to direct physical trauma or impactful force to a body part. Such incidents often occur with road traffic collisions, assaults, and sports-related injuries, and are notably common among the elderly who experience falls.
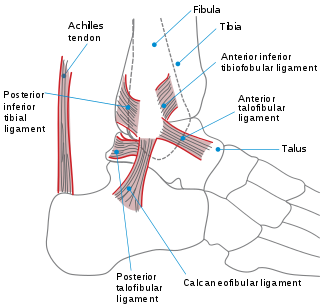
A sprained ankle is an injury where sprain occurs on one or more ligaments of the ankle. It is the most commonly occurring injury in sports, mainly in ball sports such as basketball, volleyball, football, pickleball, and tennis.

Suspension trauma, also known as orthostatic shock while suspended, harness hang syndrome (HHS), suspension syndrome, or orthostatic intolerance, is an effect which occurs when the human body is held upright without any movement for a period of time. If the person is strapped into a harness or tied to an upright object they will eventually suffer the central ischaemic response. Fainting while remaining vertical increases the risk of death from cerebral hypoxia. Since there is no evidence that these effects are specifically due to trauma, or caused by the harness itself, climbing medicine authorities have argued against the terminology of suspension trauma or harness hang syndrome and instead termed this simply "suspension syndrome".

Cerebral venous sinus thrombosis (CVST), cerebral venous and sinus thrombosis or cerebral venous thrombosis (CVT), is the presence of a blood clot in the dural venous sinuses, the cerebral veins, or both. Symptoms may include severe headache, visual symptoms, any of the symptoms of stroke such as weakness of the face and limbs on one side of the body, and seizures, which occur in around 40% of patients.

Tricyclic antidepressant overdose is poisoning caused by excessive medication of the tricyclic antidepressant (TCA) type. Symptoms may include elevated body temperature, blurred vision, dilated pupils, sleepiness, confusion, seizures, rapid heart rate, and cardiac arrest. If symptoms have not occurred within six hours of exposure they are unlikely to occur.
Permissive hypotension or hypotensive resuscitation is the use of restrictive fluid therapy, specifically in the trauma patient, that increases systemic blood pressure without reaching normotension. The goal blood pressure for these patients is a mean arterial pressure of 40-50 mmHg or systolic blood pressure of less than or equal to 80. This goes along with certain clinical criteria. Following traumatic injury, some patients experience hypotension that is usually due to blood loss (hemorrhage) but can be due to other causes as well. In the past, physicians were very aggressive with fluid resuscitation to try to bring the blood pressure to normal values. Recent studies have found that there is some benefit to allowing specific patients to experience some degree of hypotension in certain settings. This concept does not exclude therapy by means of i.v. fluid, inotropes or vasopressors, the only restriction is to avoid completely normalizing blood pressure in a context where blood loss may be enhanced. When a person starts to bleed the body starts a natural coagulation process that eventually stops the bleed. Issues with fluid resuscitation without control of bleeding are thought to be secondary to dislodgement of the thrombus that is helping to control further bleeding. Thrombus dislodgement was found to occur at a systolic pressure greater than 80mm Hg. In addition, fluid resuscitation will dilute coagulation factors that help form and stabilize a clot, hence making it harder for the body to use its natural mechanisms to stop the bleeding. These factors are aggravated by hypothermia.
References
- ↑ Thomassen; et al. (2009). "Does the horizontal position increase risk of rescue death following suspension trauma?". Emerg Med J. 26 (12): 896–8. doi:10.1136/emj.2008.064931. PMID 19934143. S2CID 21811493.
- 1 2 Adisesh, Lee, Porter (2011). "Harness suspension and first aid management: development of an evidence-based guideline". Emerg Med J. 28 (4): 265–8. doi:10.1136/emj.2010.097246. PMID 20961926. S2CID 206939778.
{{cite journal}}: CS1 maint: multiple names: authors list (link)