Cause
| | This section is empty. You can help by adding to it. (October 2024) |
| Riboflavin-responsive exercise intolerance |
|---|
Riboflavin-responsive exercise intolerance (SLC25A32 deficiency) is a rare disorder caused by mutations of the SLC25A32 gene that encodes the mitochondrial folate transporter. Patients suffer from exercise intolerance and may have disrupted motor function.
A positive correlation between SLC25A32 dysfunction and flavoenzyme deficiency has been observed suggesting that SLC25A32 is in fact a mitochondrial FAD transporter. In mice studies, besides β-oxidation and amino acid metabolism being impaired by mitochondrial FAD deficiency, Slc25a32 wipeout embryos experienced dysfunction of the glycine cleavage system– dihydrolipoamide dehydrogenase. This dihydrolipoamide dehydrogenase dysfunction disrupted folate-mediated one-carbon metabolism, leading a deficiency of 5-methyltetrahydrofolate. [1]
Patients suffer from exercise intolerance and may also have neuromuscular symptoms such as ataxia, dysarthia and muscle weakness. Staining of skeletal muscle samples with hematoxylin and eosin may reveal the ragged red fibers sign indicating disrupted mitochondrial function. In some patients, hypoketotic hypoglycemia was described. [2]
| | This section is empty. You can help by adding to it. (October 2024) |
Treatment with riboflavin, 5-formyltetrahydrofolate (Folinic acid) and/or L-5-methyltetrahydrofolate (5-MTHF) may lead to a drastic improvement of symptoms. Pyridoxal - 5 - Phosphate (P5P), a cofactor for the enzyme Serine hydroxymethyltransferase, may also assist with the conversion of tetrahydrofolate (THF) to 5,10-Methylenetetrahydrofolate (5,10-CH2-THF) a direct precursor to L-5-methyltetrahydrofolate (5-MTHF).
Riboflavin - responsive exercise intolerance was first described in 2016 by Schiff et al. [3]

Riboflavin, also known as vitamin B2, is a vitamin found in food and sold as a dietary supplement. It is essential to the formation of two major coenzymes, flavin mononucleotide and flavin adenine dinucleotide. These coenzymes are involved in energy metabolism, cellular respiration, and antibody production, as well as normal growth and development. The coenzymes are also required for the metabolism of niacin, vitamin B6, and folate. Riboflavin is prescribed to treat corneal thinning, and taken orally, may reduce the incidence of migraine headaches in adults.

Folate, also known as vitamin B9 and folacin, is one of the B vitamins. Manufactured folic acid, which is converted into folate by the body, is used as a dietary supplement and in food fortification as it is more stable during processing and storage. Folate is required for the body to make DNA and RNA and metabolise amino acids necessary for cell division and maturation of blood cells. As the human body cannot make folate, it is required in the diet, making it an essential nutrient. It occurs naturally in many foods. The recommended adult daily intake of folate in the U.S. is 400 micrograms from foods or dietary supplements.

Methylenetetrahydrofolate reductase (MTHFR) is the rate-limiting enzyme in the methyl cycle, and it is encoded by the MTHFR gene. Methylenetetrahydrofolate reductase catalyzes the conversion of 5,10-methylenetetrahydrofolate to 5-methyltetrahydrofolate, a cosubstrate for homocysteine remethylation to methionine. Natural variation in this gene is common in otherwise healthy people. Although some variants have been reported to influence susceptibility to occlusive vascular disease, neural tube defects, Alzheimer's disease and other forms of dementia, colon cancer, and acute leukemia, findings from small early studies have not been reproduced. Some mutations in this gene are associated with methylenetetrahydrofolate reductase deficiency. Complex I deficiency with recessive spastic paraparesis has also been linked to MTHFR variants. In addition, the aberrant promoter hypermethylation of this gene is associated with male infertility and recurrent spontaneous abortion.
In biochemistry and metabolism, beta oxidation (also β-oxidation) is the catabolic process by which fatty acid molecules are broken down in the cytosol in prokaryotes and in the mitochondria in eukaryotes to generate acetyl-CoA. Acetyl-CoA enters the citric acid cycle, generating NADH and FADH2, which are electron carriers used in the electron transport chain. It is named as such because the beta carbon of the fatty acid chain undergoes oxidation and is converted to a carbonyl group to start the cycle all over again. Beta-oxidation is primarily facilitated by the mitochondrial trifunctional protein, an enzyme complex associated with the inner mitochondrial membrane, although very long chain fatty acids are oxidized in peroxisomes.

Systemic primary carnitine deficiency (SPCD) is an inborn error of fatty acid transport caused by a defect in the transporter responsible for moving carnitine across the plasma membrane. Carnitine is an important amino acid for fatty acid metabolism. When carnitine cannot be transported into tissues, fatty acid oxidation is impaired, leading to a variety of symptoms such as chronic muscle weakness, cardiomyopathy, hypoglycemia and liver dysfunction. The specific transporter involved with SPCD is OCTN2, coded for by the SLC22A5 gene located on chromosome 5. SPCD is inherited in an autosomal recessive manner, with mutated alleles coming from both parents.

Mitochondrial myopathies are types of myopathies associated with mitochondrial disease. Adenosine triphosphate (ATP), the chemical used to provide energy for the cell, cannot be produced sufficiently by oxidative phosphorylation when the mitochondrion is either damaged or missing necessary enzymes or transport proteins. With ATP production deficient in mitochondria, there is an over-reliance on anaerobic glycolysis which leads to lactic acidosis either at rest or exercise-induced.

Methionine synthase (MS, MeSe, MTR) is primarily responsible for the regeneration of methionine from homocysteine in most individuals. In humans it is encoded by the MTR gene (5-methyltetrahydrofolate-homocysteine methyltransferase). Methionine synthase forms part of the S-adenosylmethionine (SAMe) biosynthesis and regeneration cycle, and is the enzyme responsible for linking the cycle to one-carbon metabolism via the folate cycle. There are two primary forms of this enzyme, the Vitamin B12 (cobalamin)-dependent (MetH) and independent (MetE) forms, although minimal core methionine synthases that do not fit cleanly into either category have also been described in some anaerobic bacteria. The two dominant forms of the enzymes appear to be evolutionary independent and rely on considerably different chemical mechanisms. Mammals and other higher eukaryotes express only the cobalamin-dependent form. In contrast, the distribution of the two forms in Archaeplastida (plants and algae) is more complex. Plants exclusively possess the cobalamin-independent form, while algae have either one of the two, depending on species. Many different microorganisms express both the cobalamin-dependent and cobalamin-independent forms.
Glutaric acidemia type 2 is an autosomal recessive metabolic disorder that is characterised by defects in the ability of the body to use proteins and fats for energy. Incompletely processed proteins and fats can build up, leading to a dangerous chemical imbalance called acidosis. It is a metabolic myopathy, categorized under fatty acid metabolism disorder as that is the bioenergetic system that it affects the most. It also affects choline metabolism.

Folate deficiency, also known as vitamin B9 deficiency, is a low level of folate and derivatives in the body. This may result in megaloblastic anemia in which red blood cells become abnormally large, and folate deficiency anemia is the term given for this medical condition. Signs of folate deficiency are often subtle. Symptoms may include fatigue, heart palpitations, shortness of breath, feeling faint, open sores on the tongue, loss of appetite, changes in the color of the skin or hair, irritability, and behavioral changes. Temporary reversible infertility may occur. Folate deficiency anemia during pregnancy may give rise to the birth of low weight birth premature infants and infants with neural tube defects.
Acyl-CoA dehydrogenases (ACADs) are a class of enzymes that function to catalyze the initial step in each cycle of fatty acid β-oxidation in the mitochondria of cells. Their action results in the introduction of a trans double-bond between C2 (α) and C3 (β) of the acyl-CoA thioester substrate. Flavin adenine dinucleotide (FAD) is a required co-factor in addition to the presence of an active site glutamate in order for the enzyme to function.

Dihydrolipoamide dehydrogenase (DLD), also known as dihydrolipoyl dehydrogenase, mitochondrial, is an enzyme that in humans is encoded by the DLD gene. DLD is a flavoprotein enzyme that oxidizes dihydrolipoamide to lipoamide.

Levomefolic acid (INN, also known as L-5-MTHF, L-methylfolate and L-5-methyltetrahydrofolate and (6S)-5-methyltetrahydrofolate, and (6S)-5-MTHF) is the primary biologically active form of folate used at the cellular level for DNA reproduction, the cysteine cycle and the regulation of homocysteine. It is also the form found in circulation and transported across membranes into tissues and across the blood–brain barrier. In the cell, L-methylfolate is used in the methylation of homocysteine to form methionine and tetrahydrofolate (THF). THF is the immediate acceptor of one carbon unit for the synthesis of thymidine-DNA, purines (RNA and DNA) and methionine. The un-methylated form, folic acid (vitamin B9), is a synthetic form of folate, and must undergo enzymatic reduction by dihydrofolate reductase (DHFR) to become biologically active.

5,10-Methylenetetrahydrofolate (N5,N10-Methylenetetrahydrofolate; 5,10-CH2-THF) is cofactor in several biochemical reactions. It exists in nature as the diastereoisomer [6R]-5,10-methylene-THF.

Electron-transferring-flavoprotein dehydrogenase is an enzyme that transfers electrons from electron-transferring flavoprotein in the mitochondrial matrix, to the ubiquinone pool in the inner mitochondrial membrane. It is part of the electron transport chain. The enzyme is found in both prokaryotes and eukaryotes and contains a flavin and FE-S cluster. In humans, it is encoded by the ETFDH gene. Deficiency in ETF dehydrogenase causes the human genetic disease multiple acyl-CoA dehydrogenase deficiency.

Inborn errors of carbohydrate metabolism are inborn error of metabolism that affect the catabolism and anabolism of carbohydrates.
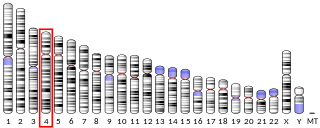
NAD-dependent methylenetetrahydrofolate dehydrogenase 2-like protein (MTHFD2L), also known as bifunctional methylenetetrahydrofolate dehydrogenase/cyclohydrolase 2, is an enzyme that in humans is encoded by the MTHFD2L gene on chromosome 4. This enzyme localizes to the inner mitochondrial membrane, where it performs the NADP+-dependent dehydrogenase/cyclohydrolase activity as part of the mitochondrial pathway to convert folate to formate. It is associated with fluctuations in cytokine secretion in response to viral infections and vaccines.

Cerebral folate deficiency is a condition in which concentrations of 5-methyltetrahydrofolate are low in the brain as measured in the cerebral spinal fluid despite being normal in the blood. Symptoms typically appear at about 5 to 24 months of age. Without treatment there may be poor muscle tone, trouble with coordination, trouble talking, and seizures.

Mitochondrial complex II deficiency, also called CII deficiency, is a rare mitochondrial disease caused by deficiency of mitochondrial complex II, also known as Succinate dehydrogenase (SDH). SDH plays a key role in metabolism; the catalytic end, made up of SDHA and SDHB oxidizes succinate to fumarate in the tricarboxylic acid (TCA) cycle. The electrons from this reaction then reduce FAD to FADH2, which ultimately reduces ubiquinone to ubiquinol in the mitochondrial electron transport chain. As of 2020, about 61 cases have been reported with genetic studies, but there are also documented cases of CII deficiencies as determined by biochemical and histological analysis without genetic studies.

5,10-Methenyltetrahydrofolate synthetase deficiency is a rare neurodevelopmental disorder caused by mutations affecting the MTHFS gene, which encodes the enzyme 5,10-Methenyltetrahydrofolate synthetase.
The mitochondrial folate transporter (MTF) is a transport protein that facilitates the transfer of tetrahydrofolate across the inner mitochondrial membrane. It is encoded by the SLC25A32 gene and belongs to the mitochondrial carrier superfamily.