Related Research Articles

Diphtheria is an infection caused by the bacterium Corynebacterium diphtheriae. Most infections are asymptomatic or have a mild clinical course, but in some outbreaks more than 10% of those diagnosed with the disease may die. Signs and symptoms may vary from mild to severe and usually start two to five days after exposure. Symptoms often come on fairly gradually, beginning with a sore throat and fever. In severe cases, a grey or white patch develops in the throat. This can block the airway and create a barking cough as in croup. The neck may swell in part due to enlarged lymph nodes. A form of diphtheria which involves the skin, eyes or genitals also exists. Complications may include myocarditis, inflammation of nerves, kidney problems, and bleeding problems due to low levels of platelets. Myocarditis may result in an abnormal heart rate and inflammation of the nerves may result in paralysis.

Scarlet fever is an infectious disease resulting from a group A streptococcus infection, also known as Streptococcus pyogenes. The signs and symptoms include a sore throat, fever, headaches, swollen lymph nodes, and a characteristic rash. The rash is red and feels like sandpaper and the tongue may be red and bumpy. It most commonly affects children between five and 15 years of age.

An antitoxin is an antibody with the ability to neutralize a specific toxin. Antitoxins are produced by certain animals, plants, and bacteria in response to toxin exposure. Although they are most effective in neutralizing toxins, they can also kill bacteria and other microorganisms. Antitoxins are made within organisms, and can be injected into other organisms, including humans, to treat an infectious disease. This procedure involves injecting an animal with a safe amount of a particular toxin. The animal's body then makes the antitoxin needed to neutralize the toxin. Later, blood is withdrawn from the animal. When the antitoxin is obtained from the blood, it is purified and injected into a human or other animal, inducing temporary passive immunity. To prevent serum sickness, it is often best to use an antitoxin obtained from the same species.

Pierre Paul Émile Roux FRS was a French physician, bacteriologist and immunologist. Roux was one of the closest collaborators of Louis Pasteur (1822–1895), a co-founder of the Pasteur Institute, and responsible for the institute's production of the anti-diphtheria serum, the first effective therapy for this disease. Additionally, he investigated cholera, chicken-cholera, rabies, and tuberculosis. Roux is regarded as a founder of the field of immunology.
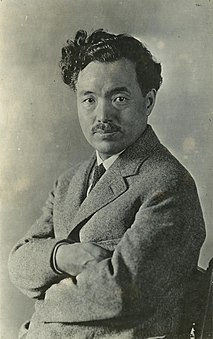
Hideyo Noguchi, also known as Seisaku Noguchi, was a prominent Japanese bacteriologist who in 1911 discovered the agent of syphilis as the cause of progressive paralytic disease.

The Pasteur Institute is a French non-profit private foundation dedicated to the study of biology, micro-organisms, diseases, and vaccines. It is named after Louis Pasteur, who invented pasteurization and vaccines for anthrax and rabies. The institute was founded on 4 June 1887, and inaugurated on 14 November 1888.
Dr. Anna Wessels Williams (1863–1954) was an American pathologist at the first municipal diagnostic laboratory in the United States. She used her medical training from the Women's Medical College of the New York Infirmary for research rather than medical practice, and over the course of her career worked on developing vaccines, treatments and diagnostic tests for many diseases, including diphtheria, rabies, scarlet fever, smallpox, influenza, and meningitis. Notably, a strain of diphtheria-causing bacteria that Williams isolated and cultivated was instrumental in producing an antitoxin to bring the disease under control. In 1932, she became the first woman to be elected chair of the laboratory section of the American Public Health Association.

Alphonse Raymond Dochez was an American physician and microbiologist. His research focused on infectious diseases, including scarlet fever, the common cold, and pneumococcal pneumonia. Dochez is credited with developing the first effective treatment for scarlet fever. His work also established viruses as the cause of the common cold.

George Frederick Dick was an American physician and bacteriologist best known for his work with scarlet fever.

Rebecca Craighill Lancefield was a prominent American microbiologist. She joined the Rockefeller Institute for Medical Research in New York in 1918, and was associated with that institute throughout her long and outstanding career. Her bibliography comprises more than 50 publications published over 60 years.
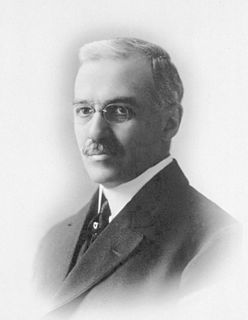
William Hallock Park was an American bacteriologist and laboratory director at the New York City Board of Health, Division of Pathology, Bacteriology, and Disinfection from 1893 to 1936.

Gladys Rowena Henry Dick was an American physician who co-developed an antitoxin and vaccine for scarlet fever with her husband, George F. Dick.

Baron Kitasato Shibasaburō was a Japanese physician and bacteriologist. He is remembered as the co-discoverer of the infectious agent of bubonic plague in Hong Kong during an outbreak in 1894, almost simultaneously with Alexandre Yersin.
Far East scarlet-like fever is an infectious disease caused by the gram negative bacillus Yersinia pseudotuberculosis. In Japan it is called Izumi fever.

Diseases and epidemics of the 19th century included long-standing epidemic threats such as smallpox, typhus, yellow fever, and scarlet fever. In addition, cholera emerged as an epidemic threat and spread worldwide in six pandemics in the nineteenth century. The third plague pandemic emerged in China in the mid-nineteenth century and spread worldwide in the 1890s.
Frederick Parker Gay was an American bacteriologist who combated typhoid fever and leprosy as well as studied the mechanism of immunity. He was a charter member of the Explorers Club.

Paul Gibier (1851–1900) was a French doctor and bacteriologist, a researcher into contagious diseases, who founded the New York Pasteur Institute. This was a pioneering private research laboratory concerned with developing bio-medical cures including vaccines and anti-toxins. He was also known for his interest in psychic phenomena.

The 1894 Hong Kong plague, part of the third plague pandemic, was a major outbreak of the bubonic plague in Hong Kong. While the plague was harshest in 1894, it returned annually between 1895 and 1929, and killed over 20,000 in total, with a fatality rate of more than 93%. The plague was a major turning point in the history of colonial Hong Kong, as it forced the colonial government to reexamine its policy towards the Chinese community, and invest in the wellbeing of the Chinese.

Ruth May Tunnicliff was an American physician, medical researcher, bacteriologist, and pathologist, based in Chicago. She developed a serum against measles, and did laboratory research for the United States Army during the 1918 influenza pandemic.

Olga Raissa Povitzky, also seen as Olga Povitsky, was a Russian-born American physician and bacteriologist with the New York Health Department; she also worked at a field hospital in France during World War I.
References
- ↑ "A Scarlet Fever Serum" (PDF). New York Times . November 3, 1902. p. 8.
- ↑ A Scarlet Fever Serum, New York Times, February 5, 1903, pg. 8.
- ↑ Scarlet Fever Serum Discovered, New York Times, February 3, 1903, pg. 9.
- ↑ A Scarlet Fever Serum, New York Times, February 5, 1903, pg. 8.
- ↑ Find Scarlet Fever Germ, New York Times, July 23, 1923, pg. 14.
- ↑ "Doctors Reveal Serum Secrets; Story of Scarlet Fever Research Work Told". Indianapolis Times . January 25, 1924. Retrieved December 15, 2021– via Chronicling America.
- ↑ Raymond Dochez, Researcher, Dies, New York Times, July 1, 1964, pg. 35.
- ↑ Cushing, H. B. Results of the Use of Scarlet Fever Antitoxin. Canadian Medical Association Journal. August, 1926, pg. 936.
- ↑ Zingher, Abraham . The Dick Test and Active Immunization With Scarlet Fever Streptococcus Toxin *. American Journal of Public Health . November, 1924, pg. 955.
- ↑ Scarlet Fever Far From Conquered, New York Times, July 23, 1930, pg. 10.