Related Research Articles

A blood type is a classification of blood, based on the presence and absence of antibodies and inherited antigenic substances on the surface of red blood cells (RBCs). These antigens may be proteins, carbohydrates, glycoproteins, or glycolipids, depending on the blood group system. Some of these antigens are also present on the surface of other types of cells of various tissues. Several of these red blood cell surface antigens can stem from one allele and collectively form a blood group system.

Blood transfusion is the process of transferring blood products into a person's circulation intravenously. Transfusions are used for various medical conditions to replace lost components of the blood. Early transfusions used whole blood, but modern medical practice commonly uses only components of the blood, such as red blood cells, white blood cells, plasma, platelets, and other clotting factors.

Amniocentesis is a medical procedure used primarily in the prenatal diagnosis of genetic conditions. It has other uses such as in the assessment of infection and fetal lung maturity. Prenatal diagnostic testing, which includes amniocentesis, is necessary to conclusively diagnose the majority of genetic disorders, with amniocentesis being the gold-standard procedure after 15 weeks' gestation.

HIV tests are used to detect the presence of the human immunodeficiency virus (HIV), the virus that causes acquired immunodeficiency syndrome (AIDS), in serum, saliva, or urine. Such tests may detect antibodies, antigens, or RNA.
Rh disease is a type of hemolytic disease of the fetus and newborn (HDFN). HDFN due to anti-D antibodies is the proper and currently used name for this disease as the Rh blood group system actually has more than 50 antigens and not only the D-antigen. The term "Rh Disease" is commonly used to refer to HDFN due to anti-D antibodies, and prior to the discovery of anti-Rho(D) immune globulin, it was the most common type of HDFN. The disease ranges from mild to severe, and occurs in the second or subsequent pregnancies of Rh-D negative women when the biologic father is Rh-D positive.

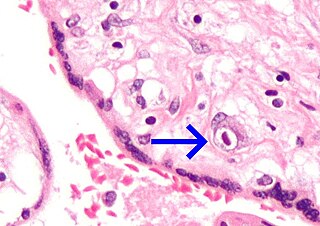
Hemolytic disease of the newborn, also known as hemolytic disease of the fetus and newborn, HDN, HDFN, or erythroblastosis fetalis, is an alloimmune condition that develops in a fetus at or around birth, when the IgG molecules produced by the mother pass through the placenta. Among these antibodies are some which attack antigens on the red blood cells in the fetal circulation, breaking down and destroying the cells. The fetus can develop reticulocytosis and anemia. The intensity of this fetal disease ranges from mild to very severe, and fetal death from heart failure can occur. When the disease is moderate or severe, many erythroblasts are present in the fetal blood, earning these forms of the disease the name erythroblastosis fetalis.

A sperm bank, semen bank, or cryobank is a facility or enterprise which purchases, stores and sells human semen. The semen is produced and sold by men who are known as sperm donors. The sperm is purchased by or for other persons for the purpose of achieving a pregnancy or pregnancies other than by a sexual partner. Sperm sold by a sperm donor is known as donor sperm.
A vertically transmitted infection is an infection caused by pathogenic bacteria or viruses that use mother-to-child transmission, that is, transmission directly from the mother to an embryo, fetus, or baby during pregnancy or childbirth. It can occur when the mother has a pre-existing disease or becomes infected during pregnancy. Nutritional deficiencies may exacerbate the risks of perinatal infections. Vertical transmission is important for the mathematical modelling of infectious diseases, especially for diseases of animals with large litter sizes, as it causes a wave of new infectious individuals.
Rho(D) immune globulin (RhIG) is a medication used to prevent RhD isoimmunization in mothers who are RhD negative and to treat idiopathic thrombocytopenic purpura (ITP) in people who are Rh positive. It is often given both during and following pregnancy. It may also be used when RhD-negative people are given RhD-positive blood. It is given by injection into muscle or a vein. A single dose lasts 12 weeks. It is made from human blood plasma.

The Rh blood group system is a human blood group system. It contains proteins on the surface of red blood cells. After the ABO blood group system, it is the most likely to be involved in transfusion reactions. The Rh blood group system consisted of 49 defined blood group antigens in 2005. As of 2023, there are over 50 antigens among which the five antigens D, C, c, E, and e are the most important. There is no d antigen. Rh(D) status of an individual is normally described with a positive (+) or negative (−) suffix after the ABO type. The terms Rh factor, Rh positive, and Rh negative refer to the Rh(D) antigen only. Antibodies to Rh antigens can be involved in hemolytic transfusion reactions and antibodies to the Rh(D) and Rh antigens confer significant risk of hemolytic disease of the newborn.
Human Immunodeficiency Virus (HIV) and Hepatitis C Virus (HCV) co-infection is a multi-faceted, chronic condition that significantly impacts public health. According to the World Health Organization (WHO), 2 to 15% of those infected with HIV are also affected by HCV, increasing their risk of morbidity and mortality due to accelerated liver disease. The burden of co-infection is especially high in certain high-risk groups, such as intravenous drug users and men who have sex with men. These individuals who are HIV-positive are commonly co-infected with HCV due to shared routes of transmission including, but not limited to, exposure to HIV-positive blood, sexual intercourse, and passage of the Hepatitis C virus from mother to infant during childbirth.
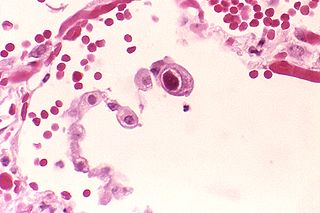
Human betaherpesvirus 5, also called human cytomegalovirus (HCMV,HHV-5), is a species of virus in the genus Cytomegalovirus, which in turn is a member of the viral family known as Herpesviridae or herpesviruses. It is also commonly called CMV. Within Herpesviridae, HCMV belongs to the Betaherpesvirinae subfamily, which also includes cytomegaloviruses from other mammals. CMV is a double-stranded DNA virus.
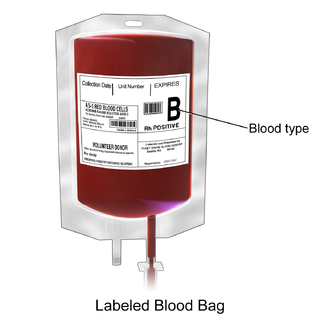
Packed red blood cells, also known as packed cells, are red blood cells that have been separated for blood transfusion. The packed cells are typically used in anemia that is either causing symptoms or when the hemoglobin is less than usually 70–80 g/L. In adults, one unit brings up hemoglobin levels by about 10 g/L. Repeated transfusions may be required in people receiving cancer chemotherapy or who have hemoglobin disorders. Cross-matching is typically required before the blood is given. It is given by injection into a vein.
A transfusion transmitted infection (TTI) is a virus, parasite, or other potential pathogen that can be transmitted in donated blood through a transfusion to a recipient. The term is usually limited to known pathogens, but also sometimes includes agents such as simian foamy virus which are not known to cause disease.
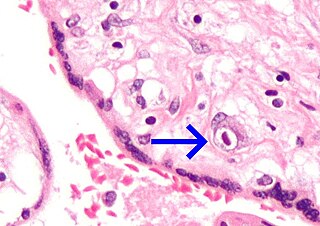
Congenital cytomegalovirus (cCMV) is cytomegalovirus (CMV) infection in a newborn baby. Most have no symptoms. Some affected babies are small. Other signs and symptoms include a rash, jaundice, hepatomegaly, retinitis, and seizures. It may lead to loss of hearing or vision, developmental disability, or a small head.
HIV in pregnancy is the presence of an HIV/AIDS infection in a woman while she is pregnant. There is a risk of HIV transmission from mother to child in three primary situations: pregnancy, childbirth, and while breastfeeding. This topic is important because the risk of viral transmission can be significantly reduced with appropriate medical intervention, and without treatment HIV/AIDS can cause significant illness and death in both the mother and child. This is exemplified by data from The Centers for Disease Control (CDC): In the United States and Puerto Rico between the years of 2014–2017, where prenatal care is generally accessible, there were 10,257 infants in the United States and Puerto Rico who were exposed to a maternal HIV infection in utero who did not become infected and 244 exposed infants who did become infected.

Neonatal infections are infections of the neonate (newborn) acquired during prenatal development or within the first four weeks of life. Neonatal infections may be contracted by mother to child transmission, in the birth canal during childbirth, or after birth. Neonatal infections may present soon after delivery, or take several weeks to show symptoms. Some neonatal infections such as HIV, hepatitis B, and malaria do not become apparent until much later. Signs and symptoms of infection may include respiratory distress, temperature instability, irritability, poor feeding, failure to thrive, persistent crying and skin rashes.
Rh factor testing, also known as Rhesus factor testing, is the procedure of determining the Rhesus D status of an individual.

Blood compatibility testing is conducted in a medical laboratory to identify potential incompatibilities between blood group systems in blood transfusion. It is also used to diagnose and prevent some complications of pregnancy that can occur when the baby has a different blood group from the mother. Blood compatibility testing includes blood typing, which detects the antigens on red blood cells that determine a person's blood type; testing for unexpected antibodies against blood group antigens ; and, in the case of blood transfusions, mixing the recipient's plasma with the donor's red blood cells to detect incompatibilities (crossmatching). Routine blood typing involves determining the ABO and RhD type, and involves both identification of ABO antigens on red blood cells and identification of ABO antibodies in the plasma. Other blood group antigens may be tested for in specific clinical situations.
In 1994, the Irish Blood Transfusion Service Board (BTSB) informed the Minister for Health that a blood product they had distributed in 1977 for the treatment of pregnant mothers had been contaminated with the hepatitis C virus. Following a report by an expert group, it was discovered that the BTSB had produced and distributed a second infected batch in 1991. The Government established a Tribunal of Inquiry to establish the facts of the case and also agreed to establish a tribunal for the compensation of victims but seemed to frustrate and delay the applications of these, in some cases terminally, ill women.
References
- 1 2 Comprehensive Donor Screening at Sperm Bank of California
- 1 2 Sims, C.; Callum, P.; Ray, M.; Iger, J.; Falk, R. (2010). "Genetic testing of sperm donors: survey of current practices". Fertility and Sterility. 94 (1): 126–129. doi: 10.1016/j.fertnstert.2009.01.139 . PMID 19342039.
- ↑ Cryos International --> Donor screening Retrieved on 20 June 2009
- ↑ Ryan KJ, Ray CG (editors) (2004). Sherris Medical Microbiology (4th ed.). McGraw Hill. pp. 556, 566–9. ISBN 0-8385-8529-9.
{{cite book}}:|author=has generic name (help) - 1 2 California Cryobank -> CMV Testing Retrieved on 12 June 2009
- ↑ First report of the absence of viral load in testicular sperm samples obtained from men with hepatitis C and HIV after washing and their subsequent use Fertility and Sterility. Volume 92, Issue 3, Pages 1012–1015 (September 2009). Nicolás Garrido, Manuel Gil-Salom, Jose M. Martínez-Jabaloyas, Marcos Meseguer
- ↑ motherearthnews.com – The Sperm Crisis