Related Research Articles

Hearing loss is a partial or total inability to hear. Hearing loss may be present at birth or acquired at any time afterwards. Hearing loss may occur in one or both ears. In children, hearing problems can affect the ability to acquire spoken language, and in adults it can create difficulties with social interaction and at work. Hearing loss can be temporary or permanent. Hearing loss related to age usually affects both ears and is due to cochlear hair cell loss. In some people, particularly older people, hearing loss can result in loneliness. Deaf people usually have little to no hearing.
Ototoxicity is the property of being toxic to the ear (oto-), specifically the cochlea or auditory nerve and sometimes the vestibular system, for example, as a side effect of a drug. The effects of ototoxicity can be reversible and temporary, or irreversible and permanent. It has been recognized since the 19th century. There are many well-known ototoxic drugs used in clinical situations, and they are prescribed, despite the risk of hearing disorders, for very serious health conditions. Ototoxic drugs include antibiotics, loop diuretics, and platinum-based chemotherapy agents. A number of nonsteroidal anti-inflammatory drugs (NSAIDS) have also been shown to be ototoxic. This can result in sensorineural hearing loss, dysequilibrium, or both. Some environmental and occupational chemicals have also been shown to affect the auditory system and interact with noise.

The auditory system is the sensory system for the sense of hearing. It includes both the sensory organs and the auditory parts of the sensory system.
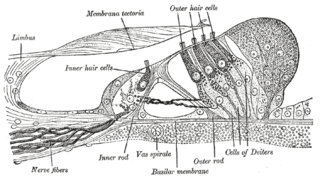
Hair cells are the sensory receptors of both the auditory system and the vestibular system in the ears of all vertebrates, and in the lateral line organ of fishes. Through mechanotransduction, hair cells detect movement in their environment.

The auditory cortex is the part of the temporal lobe that processes auditory information in humans and many other vertebrates. It is a part of the auditory system, performing basic and higher functions in hearing, such as possible relations to language switching. It is located bilaterally, roughly at the upper sides of the temporal lobes – in humans, curving down and onto the medial surface, on the superior temporal plane, within the lateral sulcus and comprising parts of the transverse temporal gyri, and the superior temporal gyrus, including the planum polare and planum temporale.
In physiology, tonotopy is the spatial arrangement of where sounds of different frequency are processed in the brain. Tones close to each other in terms of frequency are represented in topologically neighbouring regions in the brain. Tonotopic maps are a particular case of topographic organization, similar to retinotopy in the visual system.
An otoacoustic emission (OAE) is a sound that is generated from within the inner ear. Having been predicted by Austrian astrophysicist Thomas Gold in 1948, its existence was first demonstrated experimentally by British physicist David Kemp in 1978, and otoacoustic emissions have since been shown to arise through a number of different cellular and mechanical causes within the inner ear. Studies have shown that OAEs disappear after the inner ear has been damaged, so OAEs are often used in the laboratory and the clinic as a measure of inner ear health.
Auditory neuropathy (AN) is a hearing disorder in which the outer hair cells of the cochlea are present and functional, but sound information is not transmitted sufficiently by the auditory nerve to the brain. Hearing loss with AN can range from normal hearing sensitivity to profound hearing loss.
Presbycusis, or age-related hearing loss, is the cumulative effect of aging on hearing. It is a progressive and irreversible bilateral symmetrical age-related sensorineural hearing loss resulting from degeneration of the cochlea or associated structures of the inner ear or auditory nerves. The hearing loss is most marked at higher frequencies. Hearing loss that accumulates with age but is caused by factors other than normal aging is not presbycusis, although differentiating the individual effects of distinct causes of hearing loss can be difficult.

In the inner ear, stereocilia are the mechanosensing organelles of hair cells, which respond to fluid motion in numerous types of animals for various functions, including hearing and balance. They are about 10–50 micrometers in length and share some similar features of microvilli. The hair cells turn the fluid pressure and other mechanical stimuli into electric stimuli via the many microvilli that make up stereocilia rods. Stereocilia exist in the auditory and vestibular systems.

The superior olivary complex (SOC) or superior olive is a collection of brainstem nuclei that functions in multiple aspects of hearing and is an important component of the ascending and descending auditory pathways of the auditory system. The SOC is intimately related to the trapezoid body: most of the cell groups of the SOC are dorsal to this axon bundle while a number of cell groups are embedded in the trapezoid body. Overall, the SOC displays a significant interspecies variation, being largest in bats and rodents and smaller in primates.
The auditory brainstem response (ABR), also called brainstem evoked response audiometry (BERA), is an auditory evoked potential extracted from ongoing electrical activity in the brain and recorded via electrodes placed on the scalp. The measured recording is a series of six to seven vertex positive waves of which I through V are evaluated. These waves, labeled with Roman numerals in Jewett and Williston convention, occur in the first 10 milliseconds after onset of an auditory stimulus. The ABR is considered an exogenous response because it is dependent upon external factors.

Noise-induced hearing loss (NIHL) is a hearing impairment resulting from exposure to loud sound. People may have a loss of perception of a narrow range of frequencies or impaired perception of sound including sensitivity to sound or ringing in the ears. When exposure to hazards such as noise occur at work and is associated with hearing loss, it is referred to as occupational hearing loss.
The olivocochlear system is a component of the auditory system involved with the descending control of the cochlea. Its nerve fibres, the olivocochlear bundle (OCB), form part of the vestibulocochlear nerve, and project from the superior olivary complex in the brainstem (pons) to the cochlea.
Auditory fatigue is defined as a temporary loss of hearing after exposure to sound. This results in a temporary shift of the auditory threshold known as a temporary threshold shift (TTS). The damage can become permanent if sufficient recovery time is not allowed before continued sound exposure. When the hearing loss is rooted from a traumatic occurrence, it may be classified as noise-induced hearing loss, or NIHL.

A synaptopathy is a disease of the brain, spinal cord or peripheral nervous system relating to the dysfunction of synapses. This can arise as a result of a mutation in a gene encoding a synaptic protein such as an ion channel, neurotransmitter receptor, or a protein involved in neurotransmitter release. It can also arise as a result of an autoantibody targeting a synaptic protein. Synaptopathies caused by ion channel mutations are also known as synaptic channelopathies. An example is episodic ataxia. Myasthenia gravis is an example of an autoimmune synaptopathy. Some toxins also affect synaptic function. Tetanus toxin and botulinum toxin affect neurotransmitter release. Tetanus toxin can enter the body via a wound, and botulinum toxin can be ingested or administered therapeutically to alleviate dystonia or as cosmetic treatment.
D. Kent Morest, M.D., born October 4, 1934 in Kansas City, MO; died December 30, 2020 in Cambridge, MA was an American educator and researcher. He is regarded as "the father of modern neuroanatomy of the auditory system.". His unconventional use of Golgi methods to study the neuroanatomy of the auditory nervous system in humans and mammals laid the foundation for investigations into central auditory signal processing. Other notable research interests included developmental neurobiology, and the processes related to hearing loss induced by exposure to loud noises.
Edwin Rubel is an American academic and Developmental Neurobiologist holding the position of emeritus professor at the University of Washington. He was the Founding Director and first Virginia Merrill Bloedel Chair in Basic Hearing Research from 1989 to 2017.
Temporal envelope (ENV) and temporal fine structure (TFS) are changes in the amplitude and frequency of sound perceived by humans over time. These temporal changes are responsible for several aspects of auditory perception, including loudness, pitch and timbre perception and spatial hearing.
Computational audiology is a branch of audiology that employs techniques from mathematics and computer science to improve clinical treatments and scientific understanding of the auditory system. Computational audiology is closely related to computational medicine, which uses quantitative models to develop improved methods for general disease diagnosis and treatment.
References
- 1 2 3 "Sharon Kujawa, PhD". Audiology. 2014-05-23. Retrieved 2019-04-16.
- ↑ Beck M. "Can't Hear in Noisy Places? It's a Real Medical Condition". The Wall Street Journal. Retrieved 2019-04-29.
- ↑ "What's hidden in hidden hearing loss?". ENT & Audiology News. Retrieved 2019-04-16.
- ↑ Kujawa SG, Liberman MC (November 2009). "Adding insult to injury: cochlear nerve degeneration after "temporary" noise-induced hearing loss". The Journal of Neuroscience. 29 (45): 14077–85. doi:10.1523/JNEUROSCI.2845-09.2009. PMC 2812055 . PMID 19906956.
- ↑ Furman AC, Kujawa SG, Liberman MC (August 2013). "Noise-induced cochlear neuropathy is selective for fibers with low spontaneous rates". Journal of Neurophysiology. 110 (3): 577–86. doi:10.1152/jn.00164.2013. PMC 3742994 . PMID 23596328.
- ↑ "2017 Callier Prize Awarded to Sharon Kujawa". Hearing Review. 10 April 2017. Retrieved 2019-04-16.
- ↑ "2010 Academy Honors Recipients". Audiology. 2014-05-22. Retrieved 2019-04-29.
- ↑ "Distinguished Alumnus Award | Speech, Language, and Hearing Sciences". slhs.arizona.edu. Retrieved 2019-04-30.