Related Research Articles
Urinary incontinence (UI), also known as involuntary urination, is any uncontrolled leakage of urine. It is a common and distressing problem, which may have a large impact on quality of life. It has been identified as an important issue in geriatric health care. The term enuresis is often used to refer to urinary incontinence primarily in children, such as nocturnal enuresis.

Episiotomy, also known as perineotomy, is a surgical incision of the perineum and the posterior vaginal wall generally done by a midwife or obstetrician. Episiotomy is usually performed during second stage of labor to quickly enlarge the opening for the baby to pass through. The incision, which can be done from the posterior midline of the vulva straight toward the anus or at an angle to the right or left, is performed under local anesthetic, and is sutured after delivery.

A pessary is a prosthetic device inserted into the vagina for structural and pharmaceutical purposes. It is most commonly used to treat stress urinary incontinence to stop urinary leakage, and pelvic organ prolapse to maintain the location of organs in the pelvic region. It can also be used to administer medications locally in the vagina or as a method of contraception. Pessaries come in different shapes and sizes, so it is important that individuals be fitted for them by health care professionals to avoid any complications. However, there are a few instances and circumstances that allow individuals to purchase pessaries from a store without a prescription or without seeking help from a health care professional. Some side effects may occur if pessaries are not sized properly or regularly maintained, but with the appropriate care, pessaries are generally safe and well tolerated.

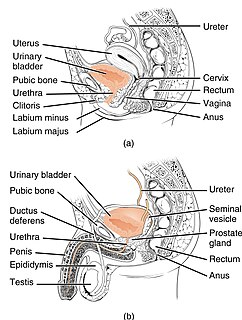
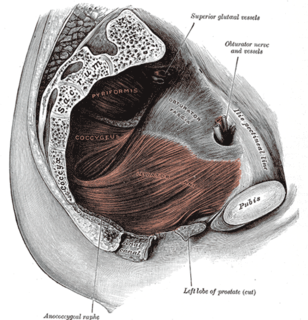
The pelvic floor or pelvic diaphragm is composed of muscle fibers of the levator ani, the coccygeus muscle, and associated connective tissue which span the area underneath the pelvis. The pelvic diaphragm is a muscular partition formed by the levatores ani and coccygei, with which may be included the parietal pelvic fascia on their upper and lower aspects. The pelvic floor separates the pelvic cavity above from the perineal region below. Both males and females have a pelvic floor. To accommodate the birth canal, a female's pelvic cavity is larger than a male's.
A rectocele or posterior vaginal wall prolapse results when the rectum herniates into or forms a bulge in the vagina. Two common causes of this defect are childbirth and hysterectomy. Rectocele also tends to occur with other forms of pelvic organ prolapse such as enterocele, sigmoidocele and cystocele.

Pelvic floor dysfunction is a term used for a variety of disorders that occur when pelvic floor muscles and ligaments are impaired. The condition affects up to 50 percent of people who have given birth. Although this condition predominantly affects individuals with ovaries, up to 16 percent of individuals with testes suffer as well. Symptoms include pelvic pain, pressure, pain during sex, urinary incontinence (UI), bowel incontinence, incomplete emptying of feces, and constipation. When pelvic organ prolapse occurs, there may be visible organ protrusion or a lump felt in the vagina or anus.
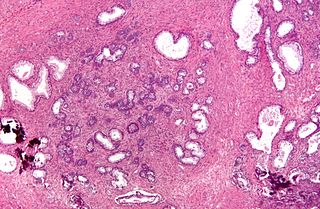
Transurethral resection of the prostate is a urological operation. It is used to treat benign prostatic hyperplasia (BPH). As the name indicates, it is performed by visualising the prostate through the urethra and removing tissue by electrocautery or sharp dissection. It has been the standard treatment for BPH for many years, but recently alternative, minimally invasive techniques have become available. This procedure is done with spinal or general anaesthetic. A triple lumen catheter is inserted through the urethra to irrigate and drain the bladder after the surgical procedure is complete. Outcome is considered excellent for 80–90% of BPH patients. The procedure carries minimal risk for erectile dysfunction, moderate risk for bleeding, and a large risk for retrograde ejaculation.
Chin augmentation using surgical implants can alter the underlying structure of the face, providing better balance to the facial features. The specific medical terms mentoplasty and genioplasty are used to refer to the reduction and addition of material to a patient's chin. This can take the form of chin height reduction or chin rounding by osteotomy, or chin augmentation using implants.

A cystocele, also known as a prolapsed bladder, is a medical condition in which a woman's bladder bulges into her vagina. Some may have no symptoms. Others may have trouble starting urination, urinary incontinence, or frequent urination. Complications may include recurrent urinary tract infections and urinary retention. Cystocele and a prolapsed urethra often occur together and is called a cystourethrocele. Cystocele can negatively affect quality of life.

Gluteoplasty denotes the plastic surgery and the liposuction procedures for the correction of the congenital, traumatic, and acquired defects and deformities of the buttocks and the anatomy of the gluteal region; and for the aesthetic enhancement of the contour of the buttocks.
Pelvic organ prolapse (POP) is characterized by descent of pelvic organs from their normal positions. In women, the condition usually occurs when the pelvic floor collapses after gynecological cancer treatment, childbirth or heavy lifting.

Radical retropubic prostatectomy is a surgical procedure in which the prostate gland is removed through an incision in the abdomen. It is most often used to treat individuals who have early prostate cancer. Radical retropubic prostatectomy can be performed under general, spinal, or epidural anesthesia and requires blood transfusion less than one-fifth of the time. Radical retropubic prostatectomy is associated with complications such as urinary incontinence and impotence, but these outcomes are related to a combination of individual patient anatomy, surgical technique, and the experience and skill of the surgeon.
Stress incontinence, also known as stress urinary incontinence (SUI) or effort incontinence is a form of urinary incontinence. It is due to inadequate closure of the bladder outlet by the urethral sphincter.
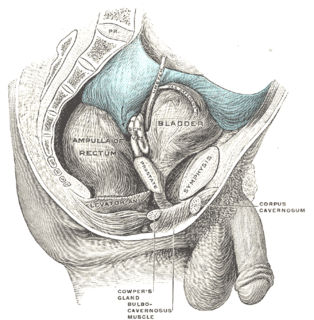
Retropubic space is a potential avascular space located between the pubic symphysis and the urinary bladder. The retropubic space is a preperitoneal space, located behind the transversalis fascia and in front of peritoneum.

The urethral sphincters are two muscles used to control the exit of urine in the urinary bladder through the urethra. The two muscles are either the male or female external urethral sphincter and the internal urethral sphincter. When either of these muscles contracts, the urethra is sealed shut.
Urogynecology or urogynaecology is a surgical sub-specialty of urology and gynecology.
In fecal incontinence (FI), surgery may be carried out if conservative measures alone are not sufficient to control symptoms. There are many surgical options described for FI, and they can be considered in 4 general groups.

Surgical mesh is a loosely woven sheet which is used as either a permanent or temporary support for organs and other tissues during surgery. Surgical mesh is created from both inorganic and biological materials and is used in a variety of surgeries. Though hernia repair surgery is the most common application, it can also be used for reconstructive work, such as in pelvic organ prolapse.
A urethral bulking injection is a gynecological procedure and medical treatment used to treat involuntary leakage of urine: urinary incontinence in women. Injectional materials are used to control stress incontinence. Bulking agents are injected into the mucosa surrounding the bladder neck and proximal urethra. This reduces the diameter of the urethra and creates resistance to urine leakage. After the procedure, the pressure forcing the urine from the bladder through the urethra is resisted by the addition of the bulking agent in the tissue surrounding the proximal urethra. Most of the time this procedure prevents urinary stress incontinence in women.

The vaginal support structures are those muscles, bones, ligaments, tendons, membranes and fascia, of the pelvic floor that maintain the position of the vagina within the pelvic cavity and allow the normal functioning of the vagina and other reproductive structures in the female. Defects or injuries to these support structures in the pelvic floor leads to pelvic organ prolapse. Anatomical and congenital variations of vaginal support structures can predispose a woman to further dysfunction and prolapse later in life. The urethra is part of the anterior wall of the vagina and damage to the support structures there can lead to incontinence and urinary retention.
References
- ↑ Arunkalaivanan, A. S.; Barrington, J. W. (2003). "Randomized trial of porcine dermal sling (Pelvicol ? Implant) vs. Tension-free Vaginal Tape (TVT) in the Surgical treatment of stress incontinence: A questionnaire-based study". International Urogynecology Journal and Pelvic Floor Dysfunction. 14 (1): 17–23, discussion 21–2. doi:10.1007/s00192-002-1000-9. PMID 12601511. S2CID 19880830.