Asbestosis is long-term inflammation and scarring of the lungs due to asbestos fibers. Symptoms may include shortness of breath, cough, wheezing, and chest tightness. Complications may include lung cancer, mesothelioma, and pulmonary heart disease.

Nail clubbing, also known as digital clubbing or clubbing, is a deformity of the finger or toe nails associated with a number of diseases, mostly of the heart and lungs. When it occurs together with joint effusions, joint pains, and abnormal skin and bone growth it is known as hypertrophic osteoarthropathy.

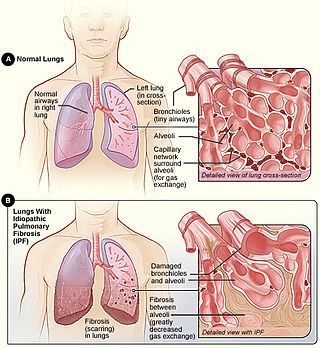
Interstitial lung disease (ILD), or diffuse parenchymal lung disease (DPLD), is a group of respiratory diseases affecting the interstitium and space around the alveoli of the lungs. It concerns alveolar epithelium, pulmonary capillary endothelium, basement membrane, and perivascular and perilymphatic tissues. It may occur when an injury to the lungs triggers an abnormal healing response. Ordinarily, the body generates just the right amount of tissue to repair damage, but in interstitial lung disease, the repair process is disrupted, and the tissue around the air sacs (alveoli) becomes scarred and thickened. This makes it more difficult for oxygen to pass into the bloodstream. The disease presents itself with the following symptoms: shortness of breath, nonproductive coughing, fatigue, and weight loss, which tend to develop slowly, over several months. The average rate of survival for someone with this disease is between three and five years. The term ILD is used to distinguish these diseases from obstructive airways diseases.

Pulmonary fibrosis is a condition in which the lungs become scarred over time. Symptoms include shortness of breath, a dry cough, feeling tired, weight loss, and nail clubbing. Complications may include pulmonary hypertension, respiratory failure, pneumothorax, and lung cancer.
Neuroendocrine hyperplasia is rare and poorly understood lung condition which is characterized by an abnormal growth pulmonary neuroendocrine cells in the lungs. It is a non-progressive disease of the interstitial tissues of the lungs. Prior to the findings of the hyperplasia of neuroendocrine cells it was known as tachypnea of infancy, as most children outgrow the need for oxygen supplementation within two to seven years. It is characterized by tachypnea, hypoxemia, and retractions. It is typically diagnosed in infants and children younger than one year of age. There is no currently recognized treatment, infants and children are given oxygen supplementation until they outgrow the need; since neuroendocrine cells do not multiply or get larger in size while the lungs continue to grow. This allows the lung disease to have less effect on lung function with age, although they will always have the same amount of neuroendocrine cells as they were born with.

Black lung disease (BLD), also known as coal-mine dust lung disease, or simply black lung, is an occupational type of pneumoconiosis caused by long-term inhalation and deposition of coal dust in the lungs and the consequent lung tissue's reaction to its presence. It is common in coal miners and others who work with coal. It is similar to both silicosis from inhaling silica dust and asbestosis from inhaling asbestos dust. Inhaled coal dust progressively builds up in the lungs and leads to inflammation, fibrosis, and in worse cases, necrosis.
Air trapping, also called gas trapping, is an abnormal retention of air in the lungs where it is difficult to exhale completely. It is observed in obstructive lung diseases such as asthma, bronchiolitis obliterans syndrome and chronic obstructive pulmonary diseases such as emphysema and chronic bronchitis.
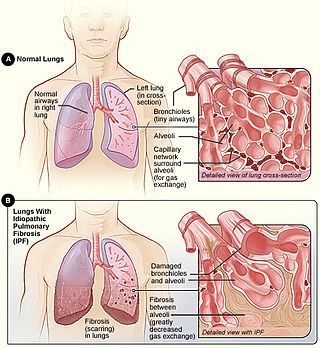
Idiopathic pulmonary fibrosis (IPF), or (formerly) fibrosing alveolitis, is a rare, progressive illness of the respiratory system, characterized by the thickening and stiffening of lung tissue, associated with the formation of scar tissue. It is a type of chronic scarring lung disease characterized by a progressive and irreversible decline in lung function. The tissue in the lungs becomes thick and stiff, which affects the tissue that surrounds the air sacs in the lungs. Symptoms typically include gradual onset of shortness of breath and a dry cough. Other changes may include feeling tired, and abnormally large and dome shaped finger and toenails. Complications may include pulmonary hypertension, heart failure, pneumonia or pulmonary embolism.

Usual interstitial pneumonia (UIP) is a form of lung disease characterized by progressive scarring of both lungs. The scarring (fibrosis) involves the pulmonary interstitium. UIP is thus classified as a form of interstitial lung disease.

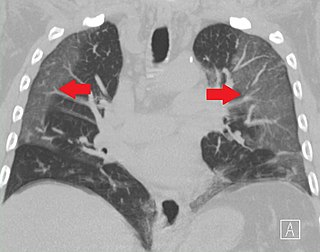
High-resolution computed tomography (HRCT) is a type of computed tomography (CT) with specific techniques to enhance image resolution. It is used in the diagnosis of various health problems, though most commonly for lung disease, by assessing the lung parenchyma. On the other hand, HRCT of the temporal bone is used to diagnose various middle ear diseases such as otitis media, cholesteatoma, and evaluations after ear operations.
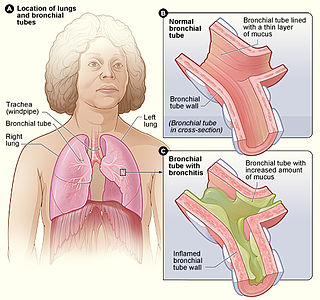
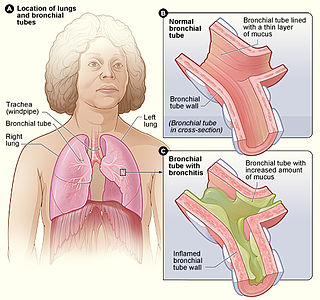
Bronchitis is inflammation of the bronchi in the lungs that causes coughing. Bronchitis usually begins as an infection in the nose, ears, throat, or sinuses. The infection then makes its way down to the bronchi. Symptoms include coughing up sputum, wheezing, shortness of breath, and chest pain. Bronchitis can be acute or chronic.

Obstructive lung disease is a category of respiratory disease characterized by airway obstruction. Many obstructive diseases of the lung result from narrowing (obstruction) of the smaller bronchi and larger bronchioles, often because of excessive contraction of the smooth muscle itself. It is generally characterized by inflamed and easily collapsible airways, obstruction to airflow, problems exhaling, and frequent medical clinic visits and hospitalizations. Types of obstructive lung disease include; asthma, bronchiectasis, bronchitis and chronic obstructive pulmonary disease (COPD). Although COPD shares similar characteristics with all other obstructive lung diseases, such as the signs of coughing and wheezing, they are distinct conditions in terms of disease onset, frequency of symptoms, and reversibility of airway obstruction. Cystic fibrosis is also sometimes included in obstructive pulmonary disease.

Idiopathic interstitial pneumonia (IIP), or noninfectious pneumonia are a class of diffuse lung diseases. These diseases typically affect the pulmonary interstitium, although some also have a component affecting the airways. There are seven recognized distinct subtypes of IIP.
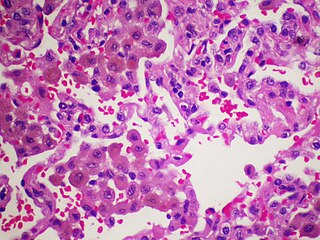
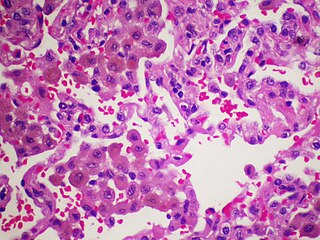
Desquamative interstitial pneumonia (DIP) is a form of idiopathic interstitial pneumonia featuring elevated numbers of macrophages within the alveoli of the lung. The alveolar macrophages have a characteristic light brown pigmentation and accumulate in the alveolar lumen and septa regions of the lower lobes of the lungs. The typical effects of the macrophage accumulation are inflammation and later fibrosis of the lung tissue.

Respiratory bronchiolitis is a lung disease associated with tobacco smoking. In pathology, it is defined by the presence of "smoker's macrophages". When manifesting significant clinical symptoms it is referred to as respiratory bronchiolitis interstitial lung disease (RB-ILD).
Combined pulmonary fibrosis and emphysema (CPFE), describes a medical syndrome involving both pulmonary fibrosis and emphysema. The combination is most commonly found in male smokers. Pulmonary function tests typically show preserved lung volume with very low transfer factor.

Chronic obstructive pulmonary disease (COPD) is a type of progressive lung disease characterized by long-term respiratory symptoms and airflow limitation. The main symptoms of COPD include shortness of breath and a cough, which may or may not produce mucus. COPD progressively worsens, with everyday activities such as walking or dressing becoming difficult. While COPD is incurable, it is preventable and treatable. The two most common types of COPD are emphysema and chronic bronchitis and have been the two classic COPD phenotypes. Emphysema is defined as enlarged airspaces (alveoli) whose walls have broken down resulting in permanent damage to the lung tissue. Chronic bronchitis is defined as a productive cough that is present for at least three months each year for two years. Both of these conditions can exist without airflow limitation when they are not classed as COPD. Emphysema is just one of the structural abnormalities that can limit airflow and can exist without airflow limitation in a significant number of people. Chronic bronchitis does not always result in airflow limitation but in young adults who smoke the risk of developing COPD is high. Many definitions of COPD in the past included emphysema and chronic bronchitis, but these have never been included in GOLD report definitions. Emphysema and chronic bronchitis remain the predominant phenotypes of COPD but there is often overlap between them and a number of other phenotypes have also been described. COPD and asthma may coexist and converge in some individuals. COPD is associated with low-grade systemic inflammation.
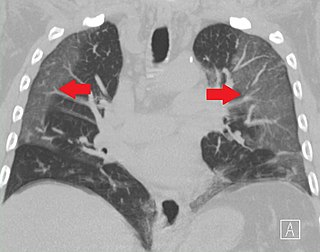
Ground-glass opacity (GGO) is a finding seen on chest x-ray (radiograph) or computed tomography (CT) imaging of the lungs. It is typically defined as an area of hazy opacification (x-ray) or increased attenuation (CT) due to air displacement by fluid, airway collapse, fibrosis, or a neoplastic process. When a substance other than air fills an area of the lung it increases that area's density. On both x-ray and CT, this appears more grey or hazy as opposed to the normally dark-appearing lungs. Although it can sometimes be seen in normal lungs, common pathologic causes include infections, interstitial lung disease, and pulmonary edema.

Emphysema is any air-filled enlargement in the body's tissues. Most commonly emphysema refers to the enlargement of air spaces (alveoli) in the lungs, and is also known as pulmonary emphysema.

Smoker’s macrophages are alveolar macrophages whose characteristics, including appearance, cellularity, phenotypes, immune response, and other functions, have been affected upon the exposure to cigarettes. These altered immune cells are derived from several signaling pathways and are able to induce numerous respiratory diseases. They are involved in asthma, chronic obstructive pulmonary diseases (COPD), pulmonary fibrosis, and lung cancer. Smoker’s macrophages are observed in both firsthand and secondhand smokers, so anyone exposed to cigarette contents, or cigarette smoke extract (CSE), would be susceptible to these macrophages, thus in turns leading to future complications.