Related Research Articles

The esophagus or oesophagus, colloquially known also as the food pipe or gullet, is an organ in vertebrates through which food passes, aided by peristaltic contractions, from the pharynx to the stomach. The esophagus is a fibromuscular tube, about 25 cm (10 in) long in adults, that travels behind the trachea and heart, passes through the diaphragm, and empties into the uppermost region of the stomach. During swallowing, the epiglottis tilts backwards to prevent food from going down the larynx and lungs. The word oesophagus is from Ancient Greek οἰσοφάγος (oisophágos), from οἴσω (oísō), future form of φέρω + ἔφαγον.

Gastroesophageal reflux disease (GERD) or gastro-oesophageal reflux disease (GORD) is one of the upper gastrointestinal chronic diseases in which stomach content persistently and regularly flows up into the esophagus, resulting in symptoms and/or complications. Symptoms include dental corrosion, dysphagia, heartburn, odynophagia, regurgitation, non-cardiac chest pain, extraesophageal symptoms such as chronic cough, hoarseness, reflux-induced laryngitis, or asthma. In the long term, and when not treated, complications such as esophagitis, esophageal stricture, and Barrett's esophagus may arise.
A hiatal hernia or hiatus hernia is a type of hernia in which abdominal organs slip through the diaphragm into the middle compartment of the chest. This may result in gastroesophageal reflux disease (GERD) or laryngopharyngeal reflux (LPR) with symptoms such as a taste of acid in the back of the mouth or heartburn. Other symptoms may include trouble swallowing and chest pains. Complications may include iron deficiency anemia, volvulus, or bowel obstruction.

Upper gastrointestinal bleeding is gastrointestinal bleeding in the upper gastrointestinal tract, commonly defined as bleeding arising from the esophagus, stomach, or duodenum. Blood may be observed in vomit or in altered form as black stool. Depending on the amount of the blood loss, symptoms may include shock.
Coffee ground vomitus refers to a particular appearance of vomit. Within organic heme molecules of red blood cells is the element iron, which oxidizes following exposure to gastric acid. This reaction causes the vomitus to look like ground coffee.

Budd–Chiari syndrome is a very rare condition, affecting one in a million adults. The condition is caused by occlusion of the hepatic veins that drain the liver. The symptoms are non-specific and vary widely, but it may present with the classical triad of abdominal pain, ascites, and liver enlargement. It is usually seen in younger adults, with the median age at diagnosis between the ages of 35 and 40, and it has a similar incidence in males and females. The syndrome can be fulminant, acute, chronic, or asymptomatic. Subacute presentation is the most common form.
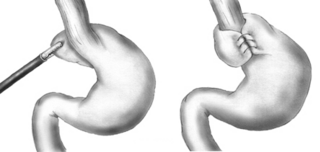
A Nissen fundoplication, or laparoscopic Nissen fundoplication when performed via laparoscopic surgery, is a surgical procedure to treat gastroesophageal reflux disease (GERD) and hiatal hernia. In GERD, it is usually performed when medical therapy has failed; but, with a Type II (paraesophageal) hiatus hernia, it is the first-line procedure. The Nissen fundoplication is total (360°), but partial fundoplications known as Thal, Belsey, Dor, Lind, and Toupet fundoplications are alternative procedures with somewhat different indications and outcomes.

Esophagogastroduodenoscopy (EGD) or oesophagogastroduodenoscopy (OGD), also called by various other names, is a diagnostic endoscopic procedure that visualizes the upper part of the gastrointestinal tract down to the duodenum. It is considered a minimally invasive procedure since it does not require an incision into one of the major body cavities and does not require any significant recovery after the procedure. However, a sore throat is common.

Esophageal varices are extremely dilated sub-mucosal veins in the lower third of the esophagus. They are most often a consequence of portal hypertension, commonly due to cirrhosis. People with esophageal varices have a strong tendency to develop severe bleeding which left untreated can be fatal. Esophageal varices are typically diagnosed through an esophagogastroduodenoscopy.

Gastric varices are dilated submucosal veins in the lining of the stomach, which can be a life-threatening cause of bleeding in the upper gastrointestinal tract. They are most commonly found in patients with portal hypertension, or elevated pressure in the portal vein system, which may be a complication of cirrhosis. Gastric varices may also be found in patients with thrombosis of the splenic vein, into which the short gastric veins that drain the fundus of the stomach flow. The latter may be a complication of acute pancreatitis, pancreatic cancer, or other abdominal tumours, as well as hepatitis C. Gastric varices and associated bleeding are a potential complication of schistosomiasis resulting from portal hypertension.

A pancreaticoduodenectomy, also known as a Whipple procedure, is a major surgical operation most often performed to remove cancerous tumours from the head of the pancreas. It is also used for the treatment of pancreatic or duodenal trauma, or chronic pancreatitis. Due to the shared blood supply of organs in the proximal gastrointestinal system, surgical removal of the head of the pancreas also necessitates removal of the duodenum, proximal jejunum, gallbladder, and, occasionally, part of the stomach.
Perioperative mortality has been defined as any death, regardless of cause, occurring within 30 days after surgery in or out of the hospital. Globally, 4.2 million people are estimated to die within 30 days of surgery each year. An important consideration in the decision to perform any surgical procedure is to weigh the benefits against the risks. Anesthesiologists and surgeons employ various methods in assessing whether a patient is in optimal condition from a medical standpoint prior to undertaking surgery, and various statistical tools are available. ASA score is the most well known of these.

Transjugular intrahepatic portosystemic shunt is an artificial channel within the liver that establishes communication between the inflow portal vein and the outflow hepatic vein. It is used to treat portal hypertension which frequently leads to intestinal bleeding, life-threatening esophageal bleeding and the buildup of fluid within the abdomen (ascites).

In medicine, a distal splenorenal shunt procedure (DSRS), also splenorenal shunt procedure and Warren shunt, is a surgical procedure in which the distal splenic vein is attached to the left renal vein. It is used to treat portal hypertension and its main complication. It was developed by W. Dean Warren.
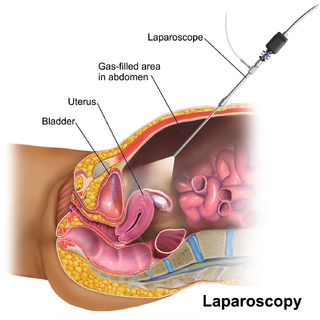
Laparoscopic hernia repair is the repair of a hiatal hernia using a laparoscope, which is a tiny telescope-like instrument. A hiatal hernia is the protrusion of an organ through its wall or cavity. There are several different methods that can be used when performing this procedure. Among them are the Nissen Fundoplication and the general laparoscopic hernia repair.

A Sengstaken–Blakemore tube is a medical device inserted through the nose or mouth and used occasionally in the management of upper gastrointestinal hemorrhage due to esophageal varices. The use of the tube was originally described in 1950, although similar approaches to bleeding varices were described by Westphal in 1930. With the advent of modern endoscopic techniques which can rapidly and definitively control variceal bleeding, Sengstaken–Blakemore tubes are rarely used at present.
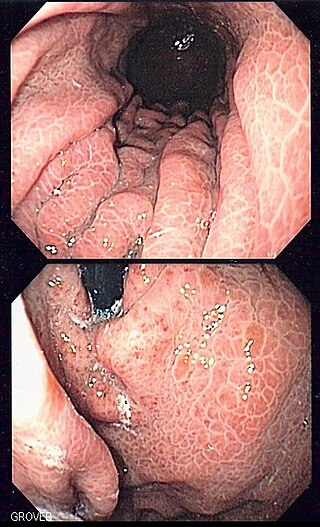
Portal hypertensive gastropathy refers to changes in the mucosa of the stomach in patients with portal hypertension; by far the most common cause of this is cirrhosis of the liver. These changes in the mucosa include friability of the mucosa and the presence of ectatic blood vessels at the surface. Patients with portal hypertensive gastropathy may experience bleeding from the stomach, which may uncommonly manifest itself in vomiting blood or melena; however, portal hypertension may cause several other more common sources of upper gastrointestinal bleeding, such as esophageal varices and gastric varices. On endoscopic evaluation of the stomach, this condition shows a characteristic mosaic or "snake-skin" appearance to the mucosa of the stomach.
Hassab's decongestion operation is an elective surgical procedure to treat esophageal varices in patients with portal hypertension as a result of cirrhosis of the liver. It was created by Dr. Mohammed Aboul-Fotouh Hassab, a professor of surgery at Alexandria University in Egypt.
Therapeutic endoscopy is the medical term for an endoscopic procedure during which treatment is carried out via the endoscope. This contrasts with diagnostic endoscopy, where the aim of the procedure is purely to visualize a part of the gastrointestinal, respiratory or urinary tract in order to aid diagnosis. In practice, a procedure which starts as a diagnostic endoscopy may become a therapeutic endoscopy depending on the findings, such as in cases of upper gastrointestinal bleeding, or the finding of polyps during colonoscopy.
Anorectal varices are the dilation of collateral submucosal vessels due to backflow in the veins of the rectum. Typically this occurs due to portal hypertension which shunts venous blood from the portal system through the portosystemic anastomosis present at this site into the systemic venous system. This can also occur in the esophagus, causing esophageal varices, and at the level of the umbilicus, causing caput medusae. Between 44% and 78% of patients with portal hypertension get anorectal varices.
References
- 1 2 Sugiura M, and Futagawa S. A new technique for treating esophageal varices. The Journal of Thoracic and Cardiovascular Surgery. 1973;66(5):677.
- 1 2 Ginsberg RJ, Waters PF, Zeldin RA, Spratt EH, Shandling B, Stone RM, and Strasberg S. A modified Sugiura procedure. The Annals of Thoracic Surgery. 1982;34(3):258-264.
- ↑ Dagenais M, Langer B, Taylor BR, and Greig PD. Experience with radical esophagogastric devascularization procedures (Sugiura) for variceal bleeding outside Japan. World J Surg. 1994;18(2):222-8.
- ↑ Mariette D, Smadja C, Borgonovo G, Grange D, and Franco D. The Sugiura procedure: a prospective experience. Surgery. 1994;115(3):282-289.
- 1 2 Belloli G, Campobasso P, and Musi L. Sugiura procedure in the surgical treatment of bleeding esophageal varices in children: Long-term results. Journal of Pediatric Surgery. 1992;27(11):1422-1426.
- ↑ Wright AS, and Rikkers LF. Current management of portal hypertension. Journal of gastrointestinal Surgery. 2005;9(7):992-1005.
- ↑ Sugiura M, and Futagawa S. Results of six hundred thirty-six esophageal transections with paraesophagogastric devascularization in the treatment of esophageal varices. J Vasc Surg. 1984, Mar;1(2):254-60.
- 1 2 Sugiura M, and Futagawa S. Further evaluation of the Sugiura procedure in the treatment of esophageal varices. Archives of Surgery. 1977;112(11):1317.
- 1 2 Selzner M, Tuttle-Newhall JE, Dahm F, Suhocki P, and Clavien PA. Current indication of a modified Sugiura procedure in the management of variceal bleeding. J Am Coll Surg. 2001, Aug;193(2):166-73.
- 1 2 3 Sugiura M, and Futagawa S. Esophageal transection with paraesophagogastric devascularizations (the Sugiura procedure) in the treatment of esophageal varices. World J Surg. 1984, Oct;8(5):673-9.
- ↑ Pierce GE, Thomas JH, and Estes NC. A transthoracic devascularization procedure for control of bleeding esophageal varices: preliminary report. Am J Surg. 1977, Dec;134(6):794-8.
- ↑ Mir J, Ponce J, Morena E, Juan M, Garrigues V, Pina R, and Berenguer J. Esophageal transection and paraesophagogastric devascularization performed as an emergency measure for uncontrolled variceal bleeding. Surg Gynecol Obstet. 1982, Dec;155(6):868-72.
- ↑ Mathur SK, Shah SR, Soonawala ZF, Karandikar SS, Nagral SS, Dalvi AN, and Mirza DF. Transabdominal extensive oesophagogastric devascularization with gastro-oesophageal stapling in the management of acute variceal bleeding. Br J Surg. 1997, Mar;84(3):413-7.
- ↑ Weese JL, Starling JR, and Yale CE. Control of bleeding esophageal varices by transabdominal esophageal transection, gastric devascularization, and splenectomy. Surg Gastroenterol. 1984;3(1):31-6.
- ↑ Barbot DJ, and Rosato EF. Experience with the esophagogastric devascularization procedure. Surgery. 1987;101(6):685-690.
- ↑ Gouge TH, and Ranson JH. Esophageal transection and paraesophagogastric devascularization for bleeding esophageal varices. The American Journal of Surgery. 1986;151(1):47-54.