Related Research Articles

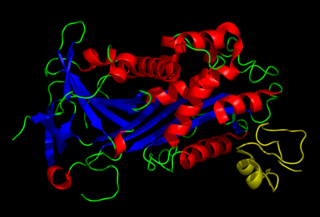
An antibody (Ab) or immunoglobulin (Ig) is a large, Y-shaped protein belonging to the immunoglobulin superfamily which is used by the immune system to identify and neutralize antigens such as bacteria and viruses, including those that cause disease. Antibodies can recognize virtually any size antigen with diverse chemical compositions from molecules. Each antibody recognizes one or more specific antigens. Antigen literally means "antibody generator", as it is the presence of an antigen that drives the formation of an antigen-specific antibody. Each tip of the "Y" of an antibody contains a paratope that specifically binds to one particular epitope on an antigen, allowing the two molecules to bind together with precision. Using this mechanism, antibodies can effectively "tag" a microbe or an infected cell for attack by other parts of the immune system, or can neutralize it directly.
Fibrinolysis is a process that prevents blood clots from growing and becoming problematic. Primary fibrinolysis is a normal body process, while secondary fibrinolysis is the breakdown of clots due to a medicine, a medical disorder, or some other cause.

Immunosuppressive drugs, also known as immunosuppressive agents, immunosuppressants and antirejection medications, are drugs that inhibit or prevent the activity of the immune system.
Humoral immunity is the aspect of immunity that is mediated by macromolecules – including secreted antibodies, complement proteins, and certain antimicrobial peptides – located in extracellular fluids. Humoral immunity is named so because it involves substances found in the humors, or body fluids. It contrasts with cell-mediated immunity. Humoral immunity is also referred to as antibody-mediated immunity.
In immunology, cytokine release syndrome (CRS) is a form of systemic inflammatory response syndrome (SIRS) that can be triggered by a variety of factors such as infections and certain drugs. It refers to cytokine storm syndromes (CSS) and occurs when large numbers of white blood cells are activated and release inflammatory cytokines, which in turn activate yet more white blood cells. CRS is also an adverse effect of some monoclonal antibody medications, as well as adoptive T-cell therapies. When occurring as a result of a medication, it is also known as an infusion reaction.
In immunology, antiserum is a blood serum containing antibodies that is used to spread passive immunity to many diseases via blood donation (plasmapheresis). For example, convalescent serum, passive antibody transfusion from a previous human survivor, used to be the only known effective treatment for ebola infection with a high success rate of 7 out of 8 patients surviving.

Hybridoma technology is a method for producing large numbers of identical antibodies, also called monoclonal antibodies. This process starts by injecting a mouse with an antigen that provokes an immune response. A type of white blood cell, the B cell, produces antibodies that bind to the injected antigen. These antibody producing B-cells are then harvested from the mouse and, in turn, fused with immortal myeloma cancer cells, to produce a hybrid cell line called a hybridoma, which has both the antibody-producing ability of the B-cell and the longevity and reproductivity of the myeloma.

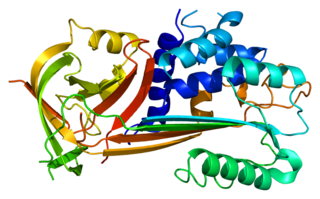
Urokinase, also known as urokinase-type plasminogen activator (uPA), is a serine protease present in humans and other animals. The human urokinase protein was discovered, but not named, by McFarlane and Pilling in 1947. Urokinase was originally isolated from human urine, and it is also present in the blood and in the extracellular matrix of many tissues. The primary physiological substrate of this enzyme is plasminogen, which is an inactive form (zymogen) of the serine protease plasmin. Activation of plasmin triggers a proteolytic cascade that, depending on the physiological environment, participates in thrombolysis or extracellular matrix degradation. This cascade had been involved in vascular diseases and cancer progression.

Anakinra, sold under the brand name Kineret, is a biopharmaceutical medication used to treat rheumatoid arthritis, cryopyrin-associated periodic syndromes, familial Mediterranean fever, and Still's disease. It is a slightly modified recombinant version of the human interleukin 1 receptor antagonist protein. It is marketed by Swedish Orphan Biovitrum. Anakinra is administered by subcutaneous injection.
Plasminogen activator inhibitor-1 (PAI-1) also known as endothelial plasminogen activator inhibitor is a protein that in humans is encoded by the SERPINE1 gene. Elevated PAI-1 is a risk factor for thrombosis and atherosclerosis.

Plasminogen activators are serine proteases that catalyze the activation of plasmin via proteolytic cleavage of its zymogen form plasminogen. Plasmin is an important factor in fibrinolysis, the breakdown of fibrin polymers formed during blood clotting. There are two main plasminogen activators: urokinase (uPA) and tissue plasminogen activator (tPA). Tissue plasminogen activators are used to treat medical conditions related to blood clotting including embolic or thrombotic stroke, myocardial infarction, and pulmonary embolism.

The Urokinase receptor, also known as urokinase plasminogen activator surface receptor (uPAR) or CD87, is a protein encoded in humans by the PLAUR gene. It is a multidomain glycoprotein tethered to the cell membrane with a glycosylphosphotidylinositol (GPI) anchor. uPAR was originally identified as a saturable binding site for urokinase on the cell surface.
Plasminogen activator inhibitor-2, a serine protease inhibitor of the serpin superfamily, is a coagulation factor that inactivates tissue plasminogen activator and urokinase. It is present in most cells, especially monocytes/macrophages. PAI-2 exists in two forms, a 60-kDa extracellular glycosylated form and a 43-kDa intracellular form.

Monoclonal antibodies (mAbs) have varied therapeutic uses. It is possible to create a mAb that binds specifically to almost any extracellular target, such as cell surface proteins and cytokines. They can be used to render their target ineffective, to induce a specific cell signal, to cause the immune system to attack specific cells, or to bring a drug to a specific cell type.
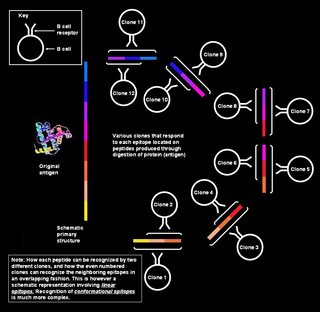
Polyclonal B cell response is a natural mode of immune response exhibited by the adaptive immune system of mammals. It ensures that a single antigen is recognized and attacked through its overlapping parts, called epitopes, by multiple clones of B cell.
A neutralizing antibody (NAb) is an antibody that defends a cell from a pathogen or infectious particle by neutralizing any effect it has biologically. Neutralization renders the particle no longer infectious or pathogenic. Neutralizing antibodies are part of the humoral response of the adaptive immune system against viruses, bacteria and microbial toxin. By binding specifically to surface structures (antigen) on an infectious particle, neutralizing antibodies prevent the particle from interacting with its host cells it might infect and destroy.
Soluble urokinase plasminogen activator receptor (suPAR) is a protein and the soluble form of uPAR. uPAR is expressed mainly on immune cells, endothelial cells, and smooth muscle cells. uPAR is a membrane-bound receptor for uPA, also known as urokinase and Vitronectin. The soluble version of uPAR, called suPAR, results from the cleavage and membrane-bound uPAR during inflammation or immune activation. The suPAR concentration is positively correlated to the activation level of the immune system. Therefore, suPAR is a marker of disease severity and aggressiveness and is associated with morbidity and mortality in several acute and chronic diseases. suPAR levels have been observed to increase with age. suPAR is present in plasma, urine, blood, serum, and cerebrospinal fluid.

Male accessory gland infection (MAGI) is a condition with signs of inflammation involving one or more sites in the male genital tract. Diagnosis is made according to parameters defined by the World Health Organization, and it is particularly made in relation to infectious or inflammatory causes of male infertility.

Jochen Reiser is a physician-scientist and a healthcare leader. He is the President of the University of Texas Medical Branch (UTMB) and CEO of the UTMB Health System, which includes the oldest medical school and nursing school in Texas. As chief executive officer, he oversees the enterprise which includes multiple campuses, five health science colleges, the Galveston National Laboratory (BSL-4) and the Correctional Health Care Services for most of Texas.

Serum B-cell maturation antigen (sBCMA) is the cleaved form of B-cell maturation antigen (BCMA), found at low levels in the serum of normal patients and generally elevated in patients with multiple myeloma (MM). Changes in sBCMA levels have been found to correlate with a MM patient’s clinical status in response to treatment.
References
- ↑ "Do You Know Your suPARnostic Level?". Virogates.com. 27 July 2009. Retrieved 12 November 2009.
- 1 2 suPAR: the molecular crystal ball. Thunø M, Macho B, Eugen-Olsen J. Dis Markers. 2009;27(3):157-72.
- 1 2 3 4 5 "What is suPAR?". virogates.com. 2020. Retrieved 7 October 2020.
- ↑ Schneider, U. V.; Nielsen, R. L.; Pedersen, C.; Eugen-Olsen, J. (2007). "The prognostic value of the suPARnostic® ELISA in HIV-1 infected individuals is not affected by uPAR promoter polymorphisms". BMC Infectious Diseases. 7: 134. doi: 10.1186/1471-2334-7-134 . PMC 2216028 . PMID 18021410.
- ↑ Rigolin, Gian Matteo et al. Soluble urokinase-type plasminogen activator receptor (suPAR) as an independent factor predicting worse prognosis and extra-bone marrow involvement in multiple myeloma patients. British Journal of Haematology. 120(60): 953–959. 18 March 2003.
- ↑ Ostrowski Sr, Ullum H, Goka BQ, Høyer-Hansen G, Obeng-Adjei G, Pedersen BK, Akanmori BD, Kurtzhals JA. 2005. Plasma concentrations of soluble urokinase-type plasminogen activator receptor are increased in patients with malaria and are associated with a poor clinical or a fatal outcome. J Infec Dis. 191(8):1331-41.
- ↑ Soluble urokinase receptor (uPAR, CD 87) is present in serum and cerebrospinal fluid in patients with neurologic diseases. Garcia-Monco JC, Coleman JL, Benach JL. 2002. Soluble urokinase receptor (uPAR, CD 87) is present in serum and cerebrospinal fluid in patients with neurologic diseases. J Neuroimmunol. 129(1-2):216-23.
- ↑ Pliyev BK, Menshikov MY. 2010. Release of the soluble urokinase-type plasminogen activator receptor (suPAR) by activated neutrophils in rheumatoid arthritis. Inflammation. 33(1):1-9.
- 1 2 3 ViroGates. "What is suPAR".
- ↑ suPARnostic Kit insert, (2008) 2nd Edition, 1-23
- 1 2 3 4 5 ViroGates. "SuPARnostic Products".
- ↑ "SuPARnostic by ViroGates".
- ↑ "suPARnostic® Products".