The pleural cavity, or pleural space, is the potential space between the pleurae of the pleural sac that surrounds each lung. A small amount of serous pleural fluid is maintained in the pleural cavity to enable lubrication between the membranes, and also to create a pressure gradient.
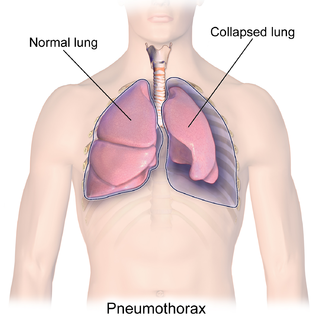
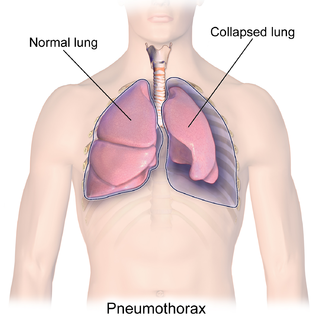
A pneumothorax is an abnormal collection of air in the pleural space between the lung and the chest wall. Symptoms typically include sudden onset of sharp, one-sided chest pain and shortness of breath. In a minority of cases, a one-way valve is formed by an area of damaged tissue, and the amount of air in the space between chest wall and lungs increases; this is called a tension pneumothorax. This can cause a steadily worsening oxygen shortage and low blood pressure. This leads to a type of shock called obstructive shock, which can be fatal unless reversed. Very rarely, both lungs may be affected by a pneumothorax. It is often called a "collapsed lung", although that term may also refer to atelectasis.

Pleurisy, also known as pleuritis, is inflammation of the membranes that surround the lungs and line the chest cavity (pleurae). This can result in a sharp chest pain while breathing. Occasionally the pain may be a constant dull ache. Other symptoms may include shortness of breath, cough, fever, or weight loss, depending on the underlying cause. Pleurisy can be caused by a variety of conditions, including viral or bacterial infections, autoimmune disorders, and pulmonary embolism.

A pleural effusion is accumulation of excessive fluid in the pleural space, the potential space that surrounds each lung. Under normal conditions, pleural fluid is secreted by the parietal pleural capillaries at a rate of 0.6 millilitre per kilogram weight per hour, and is cleared by lymphatic absorption leaving behind only 5–15 millilitres of fluid, which helps to maintain a functional vacuum between the parietal and visceral pleurae. Excess fluid within the pleural space can impair inspiration by upsetting the functional vacuum and hydrostatically increasing the resistance against lung expansion, resulting in a fully or partially collapsed lung.

Atelectasis is the partial collapse or closure of a lung resulting in reduced or absent gas exchange. It is usually unilateral, affecting part or all of one lung. It is a condition where the alveoli are deflated down to little or no volume, as distinct from pulmonary consolidation, in which they are filled with liquid. It is often referred to informally as a collapsed lung, although more accurately it usually involves only a partial collapse, and that ambiguous term is also informally used for a fully collapsed lung caused by a pneumothorax.

The mediastinum is the central compartment of the thoracic cavity. Surrounded by loose connective tissue, it is a region that contains vital organs and structures within the thorax, namely the heart and its vessels, the esophagus, the trachea, the vagus, phrenic and cardiac nerves, the thoracic duct, the thymus and the lymph nodes of the central chest.

A chest radiograph, chest X-ray (CXR), or chest film is a projection radiograph of the chest used to diagnose conditions affecting the chest, its contents, and nearby structures. Chest radiographs are the most common film taken in medicine.

A hemothorax is an accumulation of blood within the pleural cavity. The symptoms of a hemothorax may include chest pain and difficulty breathing, while the clinical signs may include reduced breath sounds on the affected side and a rapid heart rate. Hemothoraces are usually caused by an injury, but they may occur spontaneously due to cancer invading the pleural cavity, as a result of a blood clotting disorder, as an unusual manifestation of endometriosis, in response to pneumothorax, or rarely in association with other conditions.

Esophageal rupture, also known as Boerhaave syndrome, is a rupture of the esophageal wall. Iatrogenic causes account for approximately 56% of esophageal perforations, usually due to medical instrumentation such as an endoscopy or paraesophageal surgery. The 10% of esophageal perforations caused specifically by vomiting are termed Boerhaave syndrome.

Respiratory diseases, or lung diseases, are pathological conditions affecting the organs and tissues that make gas exchange difficult in air-breathing animals. They include conditions of the respiratory tract including the trachea, bronchi, bronchioles, alveoli, pleurae, pleural cavity, the nerves and muscles of respiration. Respiratory diseases range from mild and self-limiting, such as the common cold, influenza, and pharyngitis to life-threatening diseases such as bacterial pneumonia, pulmonary embolism, tuberculosis, acute asthma, lung cancer, and severe acute respiratory syndromes, such as COVID-19. Respiratory diseases can be classified in many different ways, including by the organ or tissue involved, by the type and pattern of associated signs and symptoms, or by the cause of the disease.

Pneumomediastinum is pneumatosis in the mediastinum, the central part of the chest cavity. First described in 1819 by René Laennec, the condition can result from physical trauma or other situations that lead to air escaping from the lungs, airways, or bowel into the chest cavity. In underwater divers it is usually the result of pulmonary barotrauma.

Subcutaneous emphysema occurs when gas or air accumulates and seeps under the skin, where normally no gas should be present. Subcutaneous refers to the subcutaneous tissue, and emphysema refers to trapped air pockets. Since the air generally comes from the chest cavity, subcutaneous emphysema usually occurs around the upper torso, such as on the chest, neck, face, axillae and arms, where it is able to travel with little resistance along the loose connective tissue within the superficial fascia. Subcutaneous emphysema has a characteristic crackling-feel to the touch, a sensation that has been described as similar to touching warm Rice Krispies. This sensation of air under the skin is known as subcutaneous crepitation, a form of crepitus.
Pleural disease occurs in the pleural space, which is the thin fluid-filled area in between the two pulmonary pleurae in the human body. There are several disorders and complications that can occur within the pleural area, and the surrounding tissues in the lung.

Tracheobronchial injury is damage to the tracheobronchial tree. It can result from blunt or penetrating trauma to the neck or chest, inhalation of harmful fumes or smoke, or aspiration of liquids or objects.

Fibrothorax is a medical condition characterised by severe scarring (fibrosis) and fusion of the layers of the pleural space surrounding the lungs resulting in decreased movement of the lung and ribcage. The main symptom of fibrothorax is shortness of breath. There also may be recurrent fluid collections surrounding the lungs. Fibrothorax may occur as a complication of many diseases, including infection of the pleural space known as an empyema or bleeding into the pleural space known as a haemothorax.
Double aortic arch is a relatively rare congenital cardiovascular malformation. DAA is an anomaly of the aortic arch in which two aortic arches form a complete vascular ring that can compress the trachea and/or esophagus. Most commonly there is a larger (dominant) right arch behind and a smaller (hypoplastic) left aortic arch in front of the trachea/esophagus. The two arches join to form the descending aorta which is usually on the left side. In some cases the end of the smaller left aortic arch closes and the vascular tissue becomes a fibrous cord. Although in these cases a complete ring of two patent aortic arches is not present, the term ‘vascular ring’ is the accepted generic term even in these anomalies.
The Hs and Ts is a mnemonic used to aid in remembering the possible reversible causes of cardiac arrest. A variety of disease processes can lead to a cardiac arrest; however, they usually boil down to one or more of the "Hs and Ts".

Asbestos-related diseases are disorders of the lung and pleura caused by the inhalation of asbestos fibres. Asbestos-related diseases include non-malignant disorders such as asbestosis, diffuse pleural thickening, pleural plaques, pleural effusion, rounded atelectasis and malignancies such as lung cancer and malignant mesothelioma.

The pleurae are the two flattened closed sacs filled with pleural fluid, each ensheathing each lung and lining their surrounding tissues, locally appearing as two opposing layers of serous membrane separating the lungs from the mediastinum, the inside surfaces of the surrounding chest walls and the diaphragm. Although wrapped onto itself resulting in an apparent double layer, each lung is surrounded by a single, continuous pleural membrane.

Mediastinal shift is an abnormal movement of the mediastinal structures toward one side of the chest cavity. A shift indicates a severe imbalance of pressures inside the chest. Mediastinal shifts are generally caused by increased lung volume, decreased lung volume, or abnormalities in the pleural space. Additionally, masses inside the mediastinum or musculoskeletal abnormalities can also lead to abnormal mediastinal arrangement. Typically, these shifts are observed on x-ray but also on computed tomography (CT) or magnetic resonance imaging (MRI). On chest x-ray, tracheal deviation, or movement of the trachea away from its midline position can be used as a sign of a shift. Other structures, like the heart, can also be used as reference points. Below are examples of pathologies that can cause a mediastinal shift and their appearance.