Related Research Articles

Edema, also spelled oedema, and also known as fluid retention, dropsy, hydropsy and swelling, is the build-up of fluid in the body's tissue. Most commonly, the legs or arms are affected. Symptoms may include skin which feels tight, the area may feel heavy, and joint stiffness. Other symptoms depend on the underlying cause.

Benign prostatic hyperplasia (BPH), also called prostate enlargement, is a noncancerous increase in size of the prostate gland. Symptoms may include frequent urination, trouble starting to urinate, weak stream, inability to urinate, or loss of bladder control. Complications can include urinary tract infections, bladder stones, and chronic kidney problems.
Hyponatremia or hyponatraemia is a low concentration of sodium in the blood. It is generally defined as a sodium concentration of less than 135 mmol/L (135 mEq/L), with severe hyponatremia being below 120 mEq/L. Symptoms can be absent, mild or severe. Mild symptoms include a decreased ability to think, headaches, nausea, and poor balance. Severe symptoms include confusion, seizures, and coma; death can ensue.

Cerebral edema is excess accumulation of fluid (edema) in the intracellular or extracellular spaces of the brain. This typically causes impaired nerve function, increased pressure within the skull, and can eventually lead to direct compression of brain tissue and blood vessels. Symptoms vary based on the location and extent of edema and generally include headaches, nausea, vomiting, seizures, drowsiness, visual disturbances, dizziness, and in severe cases, death.

Pulmonary edema, also known as pulmonary congestion, is excessive fluid accumulation in the tissue or air spaces of the lungs. This leads to impaired gas exchange, most often leading to dyspnea which can progress to hypoxemia and respiratory failure. Pulmonary edema has multiple causes and is traditionally classified as cardiogenic or noncardiogenic.

Uremia is the term for high levels of urea in the blood. Urea is one of the primary components of urine. It can be defined as an excess in the blood of amino acid and protein metabolism end products, such as urea and creatinine, which would be normally excreted in the urine. Uremic syndrome can be defined as the terminal clinical manifestation of kidney failure. It is the signs, symptoms and results from laboratory tests which result from inadequate excretory, regulatory, and endocrine function of the kidneys. Both uremia and uremic syndrome have been used interchangeably to denote a very high plasma urea concentration that is the result of renal failure. The former denotation will be used for the rest of the article.

Spinal anaesthesia, also called spinal block, subarachnoid block, intradural block and intrathecal block, is a form of neuraxial regional anaesthesia involving the injection of a local anaesthetic or opiod into the subarachnoid space, generally through a fine needle, usually 9 cm (3.5 in) long. It is a safe and effective form of anesthesia usually performed by anesthesiologists that can be used as an alternative to general anesthesia commonly in surgeries involving the lower extremities and surgeries below the umbilicus. The local anesthetic with or without an opioid injected into the cerebrospinal fluid provides locoregional anaesthesia: true analgesia, motor, sensory and autonomic (sympathetic) blockade. Administering analgesics in the cerebrospinal fluid without a local anaesthetic produces locoregional analgesia: markedly reduced pain sensation, some autonomic blockade, but no sensory or motor block. Locoregional analgesia, due to mainly the absence of motor and sympathetic block may be preferred over locoregional anaesthesia in some postoperative care settings. The tip of the spinal needle has a point or small bevel. Recently, pencil point needles have been made available.

Electrolyte imbalance, or water-electrolyte imbalance, is an abnormality in the concentration of electrolytes in the body. Electrolytes play a vital role in maintaining homeostasis in the body. They help to regulate heart and neurological function, fluid balance, oxygen delivery, acid–base balance and much more. Electrolyte imbalances can develop by consuming too little or too much electrolyte as well as excreting too little or too much electrolyte. Examples of electrolytes include calcium, chloride, magnesium, phosphate, potassium, and sodium.

Urinary retention is an inability to completely empty the bladder. Onset can be sudden or gradual. When of sudden onset, symptoms include an inability to urinate and lower abdominal pain. When of gradual onset, symptoms may include loss of bladder control, mild lower abdominal pain, and a weak urine stream. Those with long-term problems are at risk of urinary tract infections.
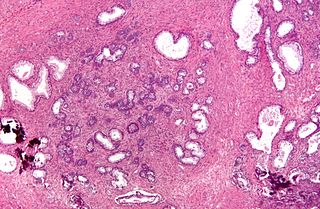
Transurethral resection of the prostate is a urological operation. It is used to treat benign prostatic hyperplasia (BPH). As the name indicates, it is performed by visualising the prostate through the urethra and removing tissue by electrocautery or sharp dissection. It has been the standard treatment for BPH for many years, but recently alternative, minimally invasive techniques have become available. This procedure is done with spinal or general anaesthetic. A triple lumen catheter is inserted through the urethra to irrigate and drain the bladder after the surgical procedure is complete. The outcome is considered excellent for 80–90% of BPH patients. The procedure carries minimal risk for erectile dysfunction, moderate risk for bleeding, and a large risk for retrograde ejaculation.

Hysteroscopy is the inspection of the uterine cavity by endoscopy with access through the cervix. It allows for the diagnosis of intrauterine pathology and serves as a method for surgical intervention.
Cardiac asthma is the medical condition of intermittent wheezing, coughing, and shortness of breath that is associated with underlying congestive heart failure (CHF). Symptoms of cardiac asthma are related to the heart's inability to effectively and efficiently pump blood in a CHF patient. This can lead to accumulation of fluid in and around the lungs, disrupting the lung's ability to oxygenate blood.

Lutembacher's syndrome is a very rare form of congenital heart disease that affects one of the chambers of the heart as well as a valve. It is commonly known as both congenital atrial septal defect (ASD) and acquired mitral stenosis (MS). Congenital atrial septal defect refers to a hole being in the septum or wall that separates the two atria; this condition is usually seen in fetuses and infants. Mitral stenosis refers to mitral valve leaflets sticking to each other making the opening for blood to pass from the atrium to the ventricles very small. With the valve being so small, blood has difficulty passing from the left atrium into the left ventricle. Septal defects that may occur with Lutembacher's syndrome include: Ostium primum atrial septal defect or ostium secundum which is more prevalent.
Jejunoileal bypass (JIB) was a surgical weight-loss procedure performed for the relief of morbid obesity from the 1950s through the 1970s in which all but 30 cm (12 in) to 45 cm (18 in) of the small bowel were detached and set to the side.
Extravasation is the leakage of a fluid out of its contained space into the surrounding area, especially blood or blood cells from vessels. In the case of inflammation, it refers to the movement of white blood cells through the capillary wall, into the surrounding tissues. This is known as. In the case of cancer metastasis, it refers to cancer cells exiting the capillaries and entering other tissues, where secondary tumors may form. The term is commonly used in a medical context.

A prostatic stent is a stent used to keep open the male urethra and allow the passing of urine in cases of prostatic obstruction and lower urinary tract symptoms (LUTS). Prostatic obstruction is a common condition with a variety of causes. Benign prostatic hyperplasia (BPH) is the most common cause, but obstruction may also occur acutely after treatment for BPH such as transurethral needle ablation of the prostate (TUNA), transurethral resection of the prostate (TURP), transurethral microwave thermotherapy (TUMT), prostate cancer or after radiation therapy.
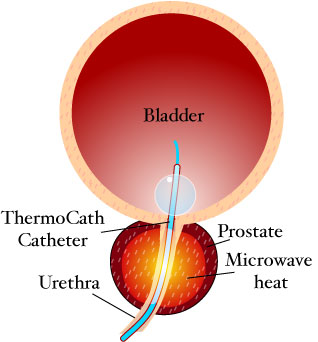
Transurethral microwave thermotherapy (TUMT) is one of a number of effective and safe procedures used in the treatment of lower urinary tract symptoms caused by benign prostatic hyperplasia. It is an alternative treatment to pharmacotherapy such as alpha blockers, transurethral resection of the prostate (TURP), transurethral needle ablation of the prostate, photoselective vaporization of the prostate and prostatic removal or prostatectomy.

Acute decompensated heart failure (ADHF) is a sudden worsening of the signs and symptoms of heart failure, which typically includes difficulty breathing (dyspnea), leg or feet swelling, and fatigue. ADHF is a common and potentially serious cause of acute respiratory distress. The condition is caused by severe congestion of multiple organs by fluid that is inadequately circulated by the failing heart. An attack of decompensation can be caused by underlying medical illness, such as myocardial infarction, an abnormal heart rhythm, infection, or thyroid disease.

Prostatic artery embolization is a non-surgical technique for treatment of benign prostatic hypertrophy (BPH).

If medical treatment is not effective, surgery may need to be performed for benign prostatic hyperplasia.
References
- ↑ Rassweiler J, Teber D, Kuntz R, Hofmann R. (20066) Complications of transurethral resection of the prostate (TURP) – incidence, management and prevention. European Urology, 50 (5): 969-980
- ↑ Hawary A, Mukhtar K, Sinclair A, Pearce I. (December 2009) “Transurethral Resection of the Prostate Syndrome: Almost Gone but not Forgotten. Journal of Endourology, 23 (12): 2013-2020
- ↑ Moorthy HK, Philip S. (2001) TURP syndrome – current concepts in the pathophysiology and management. Indian Journal of Urology, 17 (2): 97-102
- ↑ O’Donnell AM, Foo ITH. (May 2009) Anaesthesia for transurethral resection of the prostate. Continuing Education in Anaesthesia, Critical Care and Pain, 9 (3): 92-96