Related Research Articles

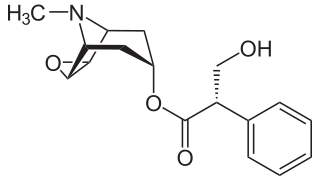
Atropine is a tropane alkaloid and anticholinergic medication used to treat certain types of nerve agent and pesticide poisonings as well as some types of slow heart rate, and to decrease saliva production during surgery. It is typically given intravenously or by injection into a muscle. Eye drops are also available which are used to treat uveitis and early amblyopia. The intravenous solution usually begins working within a minute and lasts half an hour to an hour. Large doses may be required to treat some poisonings.

The parasympathetic nervous system (PSNS) is one of the three divisions of the autonomic nervous system, the others being the sympathetic nervous system and the enteric nervous system. The enteric nervous system is sometimes considered part of the autonomic nervous system, and sometimes considered an independent system.
Baroreceptors are sensors located in the carotid sinus and in the aortic arch. They sense the blood pressure and relay the information to the brain, so that a proper blood pressure can be maintained.

Heart rate is the frequency of the heartbeat measured by the number of contractions of the heart per minute. The heart rate at which it can vary according to the body's physical needs, including the need to absorb oxygen and excrete carbon dioxide, but is also modulated by numerous factors, including genetics, physical fitness, stress or psychological status, diet, drugs, hormonal status, environment, and disease/illness as well as the interaction between and among these factors. It is usually equal or close to the pulse measured at any peripheral point.

The diving reflex, also known as the diving response and mammalian diving reflex, is a set of physiological responses to immersion that overrides the basic homeostatic reflexes, and is found in all air-breathing vertebrates studied to date. It optimizes respiration by preferentially distributing oxygen stores to the heart and brain, enabling submersion for an extended time.
Muscarinic acetylcholine receptors, or mAChRs, are acetylcholine receptors that form G protein-coupled receptor complexes in the cell membranes of certain neurons and other cells. They play several roles, including acting as the main end-receptor stimulated by acetylcholine released from postganglionic fibers in the parasympathetic nervous system.
Cushing reflex is a physiological nervous system response to increased intracranial pressure (ICP) that results in Cushing's triad of increased blood pressure, irregular breathing, and bradycardia. It is usually seen in the terminal stages of acute head injury and may indicate imminent brain herniation. It can also be seen after the intravenous administration of epinephrine and similar drugs. It was first described in detail by American neurosurgeon Harvey Cushing in 1901.

The baroreflex or baroreceptor reflex is one of the body's homeostatic mechanisms that helps to maintain blood pressure at nearly constant levels. The baroreflex provides a rapid negative feedback loop in which an elevated blood pressure causes the heart rate to decrease. Decreased blood pressure decreases baroreflex activation and causes heart rate to increase and to restore blood pressure levels. Their function is to sense pressure changes by responding to change in the tension of the arterial wall The baroreflex can begin to act in less than the duration of a cardiac cycle and thus baroreflex adjustments are key factors in dealing with postural hypotension, the tendency for blood pressure to decrease on standing due to gravity.
Labetalol is a medication used to treat high blood pressure and in long term management of angina. This includes essential hypertension, hypertensive emergencies, and hypertension of pregnancy. In essential hypertension it is generally less preferred than a number of other blood pressure medications. It can be given by mouth or by injection into a vein.
The oculocardiac reflex, also known as Aschner phenomenon, Aschner reflex, or Aschner–Dagnini reflex, is a decrease in pulse rate associated with traction applied to extraocular muscles and/or compression of the eyeball. The reflex is mediated by nerve connections between the ophthalmic branch of the trigeminal cranial nerve via the ciliary ganglion, and the vagus nerve of the parasympathetic nervous system. Nerve fibres from the maxillary and mandibular divisions of the trigeminal nerve have also been documented. These afferents synapse with the visceral motor nucleus of the vagus nerve, located in the reticular formation of the brain stem. The efferent portion is carried by the vagus nerve from the cardiovascular center of the medulla to the heart, of which increased stimulation leads to decreased output of the sinoatrial node. This reflex is especially sensitive in neonates and children, particularly during strabismus correction surgery. Oculocardiac reflex can be profound during eye examination for retinopathy of prematurity. However, this reflex may also occur with adults. Bradycardia, junctional rhythm and asystole, all of which may be life-threatening, can be induced through this reflex. This reflex has been seen to occur during many pan facial trauma surgeries due to stimulation of any of the three branches of trigeminal nerve.
The Bainbridge reflex or Bainbridge effect, also called the atrial reflex, is an increase in heart rate due to an increase in central venous pressure. Increased blood volume is detected by stretch receptors located in both sides of atria at the venoatrial junctions.
A muscarinic receptor antagonist (MRA), also called an antimuscarinic, is a type of anticholinergic agent that blocks the activity of the muscarinic acetylcholine receptor. The muscarinic receptor is a protein involved in the transmission of signals through certain parts of the nervous system, and muscarinic receptor antagonists work to prevent this transmission from occurring. Notably, muscarinic antagonists reduce the activation of the parasympathetic nervous system. The normal function of the parasympathetic system is often summarised as "rest-and-digest", and includes slowing of the heart, an increased rate of digestion, narrowing of the airways, promotion of urination, and sexual arousal. Muscarinic antagonists counter this parasympathetic "rest-and-digest" response, and also work elsewhere in both the central and peripheral nervous systems.

The muscarinic acetylcholine receptor M2, also known as the cholinergic receptor, muscarinic 2, is a muscarinic acetylcholine receptor that in humans is encoded by the CHRM2 gene. Multiple alternatively spliced transcript variants have been described for this gene. It is Gi-coupled, reducing intracellular levels of cAMP.
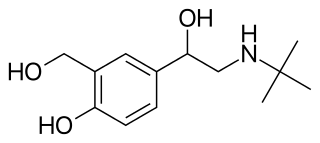
Beta adrenergic agonists or beta agonists are medications that relax muscles of the airways, causing widening of the airways and resulting in easier breathing. They are a class of sympathomimetic agents, each acting upon the beta adrenoceptors. In general, pure beta-adrenergic agonists have the opposite function of beta blockers: beta-adrenoreceptor agonist ligands mimic the actions of both epinephrine- and norepinephrine- signaling, in the heart and lungs, and in smooth muscle tissue; epinephrine expresses the higher affinity. The activation of β1, β2 and β3 activates the enzyme, adenylate cyclase. This, in turn, leads to the activation of the secondary messenger cyclic adenosine monophosphate (cAMP); cAMP then activates protein kinase A (PKA) which phosphorylates target proteins, ultimately inducing smooth muscle relaxation and contraction of the cardiac tissue.
The Bezold–Jarisch reflex involves a variety of cardiovascular and neurological processes which cause hypopnea, hypotension and bradycardia in response to noxious stimuli detected in the cardiac ventricles. The reflex is named after Albert von Bezold and Adolf Jarisch Junior. The significance of the discovery is that it was the first recognition of a chemical (non-mechanical) reflex.
Low pressure baroreceptors are baroreceptors that relay information derived from blood pressure within the autonomic nervous system. They are stimulated by stretching of the vessel wall. They are located in large systemic veins and in the walls of the atria of the heart, and pulmonary vasculature. Low pressure baroreceptors are also referred to as volume receptors and cardiopulmonary baroreceptors.
Cardiac physiology or heart function is the study of healthy, unimpaired function of the heart: involving blood flow; myocardium structure; the electrical conduction system of the heart; the cardiac cycle and cardiac output and how these interact and depend on one another.

Methoctramine is a polymethylene tetraamine that acts as a muscarinic antagonist. It preferentially binds to the pre-synaptic receptor M2, a muscarinic acetylcholine ganglionic protein complex present basically in heart cells. In normal conditions -absence of methoctramine-, the activation of M2 receptors diminishes the speed of conduction of the sinoatrial and atrioventricular nodes thus reducing the heart rate. Thanks to its apparently high cardioselectivity, it has been studied as a potential parasymphatolitic drug, particularly against bradycardia. However, currently it is only addressed for research purposes, since the administration to humans is still unavailable.
Cardiac excitation-contraction coupling (CardiacEC coupling) describes the series of events, from the production of an electrical impulse (action potential) to the contraction of muscles in the heart. This process is of vital importance as it allows for the heart to beat in a controlled manner, without the need for conscious input. EC coupling results in the sequential contraction of the heart muscles that allows blood to be pumped, first to the lungs (pulmonary circulation) and then around the rest of the body (systemic circulation) at a rate between 60 and 100 beats every minute, when the body is at rest. This rate can be altered, however, by nerves that work to either increase heart rate (sympathetic nerves) or decrease it (parasympathetic nerves), as the body's oxygen demands change. Ultimately, muscle contraction revolves around a charged atom (ion), calcium (Ca2+), which is responsible for converting the electrical energy of the action potential into mechanical energy (contraction) of the muscle. This is achieved in a region of the muscle cell, called the transverse tubule during a process known as calcium induced calcium release.
Autonomic drugs can either inhibit or enhance the functions of the parasympathetic and sympathetic nervous systems. This type of drug can be used to treat a wide range of diseases, such as glaucoma, asthma, urinary, gastrointestinal and cardiopulmonary disorders.
References
- 1 2 Doyle, D. John; Mark, Patrick W. S. (1990). "Reflex bradycardia during surgery". Canadian Journal of Anesthesia. 37 (2): 219–222. doi: 10.1007/BF03005473 . PMID 2088315.
- ↑ Deepak A. Rao; Le, Tao; Bhushan, Vikas (2007). First Aid for the USMLE Step 1 2008 (First Aid for the Usmle Step 1) . McGraw-Hill Medical. ISBN 978-0-07-149868-5. Page 254